Based on ADRIATIC Phase III trial results
which showed a 27% reduction in the risk of death versus
placebo
AstraZeneca’s IMFINZI® (durvalumab) has been approved in the US
for the treatment of adult patients with limited-stage small cell
lung cancer (LS-SCLC) whose disease has not progressed following
concurrent platinum-based chemotherapy and radiation therapy.
The approval was granted by the Food and Drug Administration
(FDA) after securing Priority Review and Breakthrough Therapy
Designation. It was based on results from the ADRIATIC Phase III
trial which were presented during the Plenary Session of the 2024
American Society of Clinical Oncology (ASCO) Annual Meeting and
subsequently published in the New England Journal of Medicine.
SCLC is a highly aggressive form of lung cancer.1 LS-SCLC
typically recurs and progresses rapidly, despite initial response
to standard-of-care chemotherapy and radiotherapy.2-3 The prognosis
for LS-SCLC is particularly poor, as only 15-30% of patients will
be alive five years after diagnosis.4
Suresh Senan, PhD, Professor of Clinical Experimental
Radiotherapy at the Amsterdam University Medical Centers, The
Netherlands, and international coordinating investigator in the
trial, said: “Durvalumab is the first and only systemic treatment
following curative-intent, platinum-based chemoradiotherapy to show
improved survival for patients with this aggressive form of lung
cancer. This finding represents the first advance for this disease
in four decades. The ADRIATIC trial showed 57 percent of patients
were still alive at three years after being treated with
durvalumab, which underscores the practice-changing potential of
this medicine in this setting.”
Dave Fredrickson, Executive Vice President, Oncology Business
Unit, AstraZeneca, said: “This approval for IMFINZI marks a
breakthrough for patients with limited-stage small cell lung
cancer, allowing them to receive immunotherapy for the first time.
The ADRIATIC trial showed an improvement in median overall survival
of 22.5 months, setting a new benchmark. IMFINZI is now the only
immunotherapy approved for both limited- and extensive-stage small
cell lung cancer, underscoring our commitment to improving survival
rates.”
Dusty Donaldson, Founder and Executive Director of LiveLung,
said: "This new treatment option is a game changer for patients
with limited-stage small cell lung cancer, a disease known for its
high rate of recurrence. Historically, more often than not,
clinical trials to identify new treatment options for this type of
cancer have failed to show benefit. We are therefore so excited
that many more people will now have the opportunity to access this
immunotherapy treatment that holds the potential to significantly
improve outcomes."
In the trial, IMFINZI reduced the risk of death by 27% versus
placebo (based on an overall survival [OS] hazard ratio [HR] of
0.73; 95% confidence interval [CI] 0.57-0.93; P=0.0104). Estimated
median OS was 55.9 months for IMFINZI versus 33.4 months for
placebo. An estimated 57% of patients treated with IMFINZI were
alive at three years compared to 48% for placebo.
IMFINZI also reduced the risk of disease progression or death by
24% (based on a progression-free survival [PFS] HR of 0.76; 95% CI
0.61-0.95; P=0.0161) versus placebo. Median PFS was 16.6 months for
IMFINZI versus 9.2 months for placebo. An estimated 46% of patients
treated with IMFINZI had not experienced disease progression at two
years compared to 34% for placebo.
The safety profile for IMFINZI was generally manageable and
consistent with the known profile of this medicine. No new safety
signals were observed.
IMFINZI is also approved in Switzerland in this setting based on
the ADRIATIC results. Regulatory applications are currently under
review in the EU, Japan and several other countries in this
indication.
IMPORTANT SAFETY INFORMATION
There are no contraindications for IMFINZI® (durvalumab).
Immune-Mediated Adverse Reactions
Important immune-mediated adverse reactions listed under
Warnings and Precautions may not include all possible severe and
fatal immune-mediated reactions. Immune-mediated adverse reactions,
which may be severe or fatal, can occur in any organ system or
tissue. Immune-mediated adverse reactions can occur at any time
after starting treatment or after discontinuation. Monitor patients
closely for symptoms and signs that may be clinical manifestations
of underlying immune-mediated adverse reactions. Evaluate liver
enzymes, creatinine, and thyroid function at baseline and
periodically during treatment. In cases of suspected
immune-mediated adverse reactions, initiate appropriate workup to
exclude alternative etiologies, including infection. Institute
medical management promptly, including specialty consultation as
appropriate. Withhold or permanently discontinue IMFINZI depending
on severity. See USPI Dosing and Administration for specific
details. In general, if IMFINZI requires interruption or
discontinuation, administer systemic corticosteroid therapy (1 mg
to 2 mg/kg/day prednisone or equivalent) until improvement to Grade
1 or less. Upon improvement to Grade 1 or less, initiate
corticosteroid taper and continue to taper over at least 1 month.
Consider administration of other systemic immunosuppressants in
patients whose immune-mediated adverse reactions are not controlled
with corticosteroid therapy.
Immune-Mediated
Pneumonitis
IMFINZI can cause immune-mediated pneumonitis. The incidence of
pneumonitis is higher in patients who have received prior thoracic
radiation. In patients who did not receive recent prior radiation,
the incidence of immune-mediated pneumonitis was 2.4% (34/1414),
including fatal (<0.1%), and Grade 3-4 (0.4%) adverse reactions.
The incidence of pneumonitis (including radiation pneumonitis) in
patients with LS-SCLC following chemoradiation within 42 days prior
to initiation of IMFINZI in ADRIATIC was 14% (37/262) in patients
receiving IMFINZI and 6% (16/265) in patients receiving placebo. Of
the patients who received IMFINZI (262), 0.4% had a fatal adverse
reaction and 2.7% had Grade 3 adverse reactions.
Immune-Mediated Colitis
IMFINZI can cause immune-mediated colitis that is frequently
associated with diarrhea. Cytomegalovirus (CMV)
infection/reactivation has been reported in patients with
corticosteroid-refractory immune-mediated colitis. In cases of
corticosteroid-refractory colitis, consider repeating infectious
workup to exclude alternative etiologies. Immune-mediated colitis
occurred in 2% (37/1889) of patients receiving IMFINZI, including
Grade 4 (<0.1%) and Grade 3 (0.4%) adverse reactions.
Immune-Mediated
Hepatitis
IMFINZI can cause immune-mediated hepatitis. Immune-mediated
hepatitis occurred in 2.8% (52/1889) of patients receiving IMFINZI,
including fatal (0.2%), Grade 4 (0.3%) and Grade 3 (1.4%) adverse
reactions.
Immune-Mediated
Endocrinopathies
- Adrenal Insufficiency: IMFINZI can cause primary or
secondary adrenal insufficiency. For Grade 2 or higher adrenal
insufficiency, initiate symptomatic treatment, including hormone
replacement as clinically indicated. Immune-mediated adrenal
insufficiency occurred in 0.5% (9/1889) of patients receiving
IMFINZI, including Grade 3 (<0.1%) adverse reactions.
- Hypophysitis: IMFINZI can cause immune-mediated
hypophysitis. Hypophysitis can present with acute symptoms
associated with mass effect such as headache, photophobia, or
visual field cuts. Hypophysitis can cause hypopituitarism. Initiate
symptomatic treatment including hormone replacement as clinically
indicated. Grade 3 hypophysitis/hypopituitarism occurred in
<0.1% (1/1889) of patients who received IMFINZI.
- Thyroid Disorders: IMFINZI can cause immune-mediated
thyroid disorders. Thyroiditis can present with or without
endocrinopathy. Hypothyroidism can follow hyperthyroidism. Initiate
hormone replacement therapy for hypothyroidism or institute medical
management of hyperthyroidism as clinically indicated.
- Thyroiditis: Immune-mediated thyroiditis occurred in
0.5% (9/1889) of patients receiving IMFINZI, including Grade 3
(<0.1%) adverse reactions.
- Hyperthyroidism: Immune-mediated hyperthyroidism
occurred in 2.1% (39/1889) of patients receiving IMFINZI.
- Hypothyroidism: Immune-mediated hypothyroidism occurred
in 8.3% (156/1889) of patients receiving IMFINZI, including Grade 3
(<0.1%) adverse reactions.
- Type 1 Diabetes Mellitus, which can present with diabetic
ketoacidosis: Monitor patients for hyperglycemia or other signs
and symptoms of diabetes. Initiate treatment with insulin as
clinically indicated. Grade 3 immune-mediated Type 1 diabetes
mellitus occurred in <0.1% (1/1889) of patients receiving
IMFINZI.
Immune-Mediated Nephritis with Renal
Dysfunction
IMFINZI can cause immune-mediated nephritis. Immune-mediated
nephritis occurred in 0.5% (10/1889) of patients receiving IMFINZI,
including Grade 3 (<0.1%) adverse reactions.
Immune-Mediated Dermatology
Reactions
IMFINZI can cause immune-mediated rash or dermatitis.
Exfoliative dermatitis, including Stevens-Johnson Syndrome (SJS),
drug rash with eosinophilia and systemic symptoms (DRESS), and
toxic epidermal necrolysis (TEN), has occurred with PD-1/L-1
blocking antibodies. Topical emollients and/or topical
corticosteroids may be adequate to treat mild to moderate
non-exfoliative rashes. Immune-mediated rash or dermatitis occurred
in 1.8% (34/1889) of patients receiving IMFINZI, including Grade 3
(0.4%) adverse reactions.
Other Immune-Mediated Adverse
Reactions
The following clinically significant, immune-mediated adverse
reactions occurred at an incidence of less than 1% each in patients
who received IMFINZI or were reported with the use of other
PD-1/PD-L1 blocking antibodies.
- Cardiac/vascular: Myocarditis, pericarditis,
vasculitis.
- Nervous system: Meningitis, encephalitis, myelitis and
demyelination, myasthenic syndrome/myasthenia gravis (including
exacerbation), Guillain-Barré syndrome, nerve paresis, autoimmune
neuropathy.
- Ocular: Uveitis, iritis, and other ocular inflammatory
toxicities can occur. Some cases can be associated with retinal
detachment. Various grades of visual impairment to include
blindness can occur. If uveitis occurs in combination with other
immune-mediated adverse reactions, consider a
Vogt-Koyanagi-Harada-like syndrome, as this may require treatment
with systemic steroids to reduce the risk of permanent vision
loss.
- Gastrointestinal: Pancreatitis including increases in
serum amylase and lipase levels, gastritis, duodenitis.
- Musculoskeletal and connective tissue disorders:
Myositis/polymyositis, rhabdomyolysis and associated sequelae
including renal failure, arthritis, polymyalgia rheumatic.
- Endocrine: Hypoparathyroidism.
- Other (hematologic/immune): Hemolytic anemia, aplastic
anemia, hemophagocytic lymphohistiocytosis, systemic inflammatory
response syndrome, histiocytic necrotizing lymphadenitis (Kikuchi
lymphadenitis), sarcoidosis, immune thrombocytopenia, solid organ
transplant rejection, other transplant (including corneal graft)
rejection.
Infusion-Related Reactions
IMFINZI can cause severe or life-threatening infusion-related
reactions. Monitor for signs and symptoms of infusion-related
reactions. Interrupt, slow the rate of, or permanently discontinue
IMFINZI based on the severity. See USPI Dosing and Administration
for specific details. For Grade 1 or 2 infusion-related reactions,
consider using pre-medications with subsequent doses.
Infusion-related reactions occurred in 2.2% (42/1889) of patients
receiving IMFINZI, including Grade 3 (0.3%) adverse reactions.
Complications of Allogeneic HSCT after IMFINZI
Fatal and other serious complications can occur in patients who
receive allogeneic hematopoietic stem cell transplantation (HSCT)
before or after being treated with a PD-1/L-1 blocking antibody.
Transplant-related complications include hyperacute
graft-versus-host disease (GVHD), acute GVHD, chronic GVHD, hepatic
veno-occlusive disease (VOD) after reduced intensity conditioning,
and steroid-requiring febrile syndrome (without an identified
infectious cause). These complications may occur despite
intervening therapy between PD-1/L-1 blockade and allogeneic HSCT.
Follow patients closely for evidence of transplant-related
complications and intervene promptly. Consider the benefit versus
risks of treatment with a PD-1/L-1 blocking antibody prior to or
after an allogeneic HSCT.
Embryo-Fetal Toxicity
Based on its mechanism of action and data from animal studies,
IMFINZI can cause fetal harm when administered to a pregnant woman.
Advise pregnant women of the potential risk to a fetus. In females
of reproductive potential, verify pregnancy status prior to
initiating IMFINZI and advise them to use effective contraception
during treatment with IMFINZI and for 3 months after the last dose
of IMFINZI.
Lactation
There is no information regarding the presence of IMFINZI in
human milk; however, because of the potential for adverse reactions
in breastfed infants from IMFINZI, advise women not to breastfeed
during treatment and for 3 months after the last dose.
Adverse Reactions
- In patients with limited-stage SCLC in the ADRIATIC study
receiving IMFINZI (n=262), the most common adverse reactions
occurring in ≥20% of patients receiving IMFINZI were pneumonitis or
radiation pneumonitis (38%), and fatigue (21%). The most common
Grade 3 or 4 adverse reactions (≥3%) were pneumonitis or radiation
pneumonitis and pneumonia.
- In patients with limited-stage SCLC in the ADRIATIC study
receiving IMFINZI (n=262), IMFINZI was permanently discontinued due
to adverse reactions in 16% of the patients receiving IMFINZI.
Serious adverse reactions occurred in 30% of patients receiving
IMFINZI. The most frequent serious adverse reactions reported in
≥1% of patients receiving IMFINZI were pneumonitis or radiation
pneumonitis (12%), and pneumonia (5%). Fatal adverse reactions
occurred in 2.7% of patients who received IMFINZI including
pneumonia (1.5%), cardiac failure, encephalopathy and pneumonitis
(0.4% each).
The safety and effectiveness of IMFINZI has not been established
in pediatric patients.
Indication:
IMFINZI® (durvalumab), as a single agent, is indicated for the
treatment of adult patients with limited-stage small cell lung
cancer (LS-SCLC) whose disease has not progressed following
concurrent platinum-based chemotherapy and radiation therapy
(cCRT).
Please see Full Prescribing Information including Medication
Guide for IMFINZI.
Notes
Small cell lung cancer
Lung cancer is the leading cause of cancer death among both men
and women, accounting for about one-fifth of all cancer deaths.5-6
Lung cancer is broadly split into non-small cell lung cancer
(NSCLC) and SCLC, with about 15% of cases classified as SCLC.7
LS-SCLC (Stage I-III) is classified as SCLC that is generally
only in one lung or one side of the chest.8 LS-SCLC accounts for
approximately 30% of SCLC diagnoses and the prognosis remains poor
despite curative-intent treatment with standard-of-care concurrent
chemoradiotherapy (cCRT).9
ADRIATIC
The ADRIATIC trial is a randomized, double-blind,
placebo-controlled, multi-center global Phase III trial evaluating
IMFINZI monotherapy and IMFINZI plus tremelimumab-actl versus
placebo in the treatment of 730 patients with LS-SCLC who had not
progressed following cCRT. In the experimental arms, patients were
randomized to receive a 1500 mg fixed dose of IMFINZI with or
without tremelimumab-actl 75 mg every four weeks for up to four
doses/cycles each, followed by IMFINZI every four weeks for up to
24 months.
The dual primary endpoints were PFS and OS for IMFINZI
monotherapy versus placebo. Key secondary endpoints included OS and
PFS for IMFINZI plus tremelimumab-actl versus placebo, safety and
quality of life measures. The trial included 164 centers in 19
countries across North and South America, Europe and Asia.
IMFINZI
IMFINZI® (durvalumab) is a human monoclonal antibody that binds
to the PD-L1 protein and blocks the interaction of PD-L1 with the
PD-1 and CD80 proteins, countering the tumor's immune-evading
tactics and releasing the inhibition of immune responses.
In addition to its indication in LS-SCLC, IMFINZI is the only
approved immunotherapy and the global standard of care in the
curative-intent setting of unresectable, Stage III NSCLC in
patients whose disease has not progressed after CRT. Additionally,
IMFINZI is approved as a perioperative treatment in combination
with neoadjuvant chemotherapy in resectable NSCLC, in combination
with chemotherapy (etoposide and either carboplatin or cisplatin)
for the treatment of extensive-stage SCLC, and in combination with
a short course of tremelimumab-actl and chemotherapy for the
treatment of metastatic NSCLC.
IMFINZI is also approved in combination with chemotherapy
(gemcitabine plus cisplatin) in locally advanced or metastatic
biliary tract cancer and in combination with tremelimumab-actl in
unresectable hepatocellular carcinoma (HCC). IMFINZI is also
approved as a monotherapy in unresectable HCC in Japan and the
EU.
IMFINZI is also approved in combination with chemotherapy
(carboplatin and paclitaxel) followed by IMFINZI monotherapy in
primary advanced or recurrent endometrial cancer that is mismatch
repair deficient (dMMR) in the US. In the EU, IMFINZI plus
chemotherapy followed by olaparib and IMFINZI is approved for
patients with mismatch repair proficient (pMMR) advanced or
recurrent endometrial cancer, and IMFINZI plus chemotherapy
followed by IMFINZI alone is approved for patients with dMMR
disease. In Japan, IMFINZI plus chemotherapy followed by IMFINZI
monotherapy has also been approved as 1st-line treatment in primary
advanced or recurrent endometrial cancer, and IMFINZI plus
chemotherapy followed by IMFINZI and olaparibhas been approved for
patients with pMMR disease.
IMFINZI is also under review by global regulatory authorities as
perioperative treatment in combination with neoadjuvant
chemotherapy based on the results of the NIAGARA Phase III trial,
which demonstrated a statistically significant and clinically
meaningful improvement in the primary endpoint of event-free
survival and the key secondary endpoint of OS versus neoadjuvant
chemotherapy.
Since the first approval in May 2017, more than 374,000 patients
have been treated with IMFINZI. As part of a broad development
program, IMFINZI is being tested as a single treatment and in
combinations with other anti-cancer treatments for patients with
SCLC, NSCLC, breast cancer, bladder cancer, several
gastrointestinal and gynecologic cancers, and other solid
tumors.
AstraZeneca in lung cancer
AstraZeneca is working to bring patients with lung cancer closer
to cure through the detection and treatment of early-stage disease,
while also pushing the boundaries of science to improve outcomes in
the resistant and advanced settings. By defining new therapeutic
targets and investigating innovative approaches, the Company aims
to match medicines to the patients who can benefit most.
The Company’s comprehensive portfolio includes leading lung
cancer medicines and the next wave of innovations, including
osimertinib and gefitinib; IMFINZI and tremelimumab-actl;
fam-trastuzumab deruxtecan-nxki and datopotamab deruxtecan in
collaboration with Daiichi Sankyo; savolitinib in collaboration
with HUTCHMED; as well as a pipeline of potential new medicines and
combinations across diverse mechanisms of action.
AstraZeneca is a founding member of the Lung Ambition Alliance,
a global coalition working to accelerate innovation and deliver
meaningful improvements for people with lung cancer, including and
beyond treatment.
AstraZeneca in immuno-oncology (IO)
AstraZeneca is a pioneer in introducing the concept of
immunotherapy into dedicated clinical areas of high unmet medical
need. The Company has a comprehensive and diverse IO portfolio and
pipeline anchored in immunotherapies designed to overcome evasion
of the anti-tumor immune response and stimulate the body’s immune
system to attack tumors.
AstraZeneca strives to redefine cancer care and help transform
outcomes for patients with IMFINZI as a monotherapy and in
combination with tremelimumab-actl as well as other novel
immunotherapies and modalities. The Company is also investigating
next-generation immunotherapies like bispecific antibodies and
therapeutics that harness different aspects of immunity to target
cancer, including cell therapy and T-cell engagers.
AstraZeneca is pursuing an innovative clinical strategy to bring
IO-based therapies that deliver long-term survival to new settings
across a wide range of cancer types. The Company is focused on
exploring novel combination approaches to help prevent treatment
resistance and drive longer immune responses. With an extensive
clinical program, the Company also champions the use of IO
treatment in earlier disease stages, where there is the greatest
potential for cure.
AstraZeneca in oncology
AstraZeneca is leading a revolution in oncology with the
ambition to provide cures for cancer in every form, following the
science to understand cancer and all its complexities to discover,
develop and deliver life-changing medicines to patients.
The Company's focus is on some of the most challenging cancers.
It is through persistent innovation that AstraZeneca has built one
of the most diverse portfolios and pipelines in the industry, with
the potential to catalyze changes in the practice of medicine and
transform the patient experience.
AstraZeneca has the vision to redefine cancer care and, one day,
eliminate cancer as a cause of death.
AstraZeneca
AstraZeneca is a global, science-led biopharmaceutical company
that focuses on the discovery, development, and commercialization
of prescription medicines in Oncology, Rare Diseases, and
BioPharmaceuticals, including Cardiovascular, Renal &
Metabolism, and Respiratory & Immunology. Based in Cambridge,
UK, AstraZeneca operates in over 125 countries, and its innovative
medicines are used by millions of patients worldwide. For more
information, please visit www.astrazeneca-us.com and follow us on
social media @AstraZeneca.
References
- National Cancer Institute. NCI dictionary - small cell lung
cancer. Accessed December 4, 2024. Available at:
https://www.cancer.gov/publications/dictionaries/cancer-terms/def/small-cell-lung-cancer.
- Qin A, Kalemkerian GP. Treatment options for relapsed
small-cell lung cancer: what progress have we made? J Oncol Pract.
2018;14(6):369-370.
- Cheng Y, et al. Durvalumab after chemoradiotherapy in
limited-stage small-cell lung cancer. N Engl J Med.
2024;391(14):1313-1327.
- Bebb DG, et al. Symptoms and Experiences with small cell lung
cancer: a mixed methods study of patients and caregivers. Pulm
Ther. 2023;9:435-450.
- World Health Organization. International Agency for Research on
Cancer. Lung Fact Sheet. Accessed December 4, 2024. Available at:
https://gco.iarc.who.int/today/en/fact-sheets-cancers.
- World Health Organization. International agency for research on
cancer world fact sheet. Accessed December 4, 2024. Available at:
https://gco.iarc.who.int/media/globocan/factsheets/populations/900-world-fact-sheet.pdf.
- LUNGevity Foundation. Types of lung cancer. Accessed December
4, 2024. Available at:
https://www.lungevity.org/for-patients-caregivers/lung-cancer-101/types-of-lung-cancer.
- American Cancer Society. Small cell lung cancer stages.
Accessed December 4, 2024. Available at:
https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/staging-sclc.html.
- Senan S, et al. ADRIATIC: A phase III trial of durvalumab ±
tremelimumab after concurrent chemoradiation for patients with
limited stage small cell lung cancer. Ann Oncol. 2019;30(suppl.
2):ii25.
US-96374 Last Updated 12/24
View source
version on businesswire.com: https://www.businesswire.com/news/home/20241205473309/en/
Media Inquiries Brendan McEvoy +1 302 885 2677 Chelsea
Tressler +1 302 885 2677
US Media Mailbox: usmediateam@astrazeneca.com
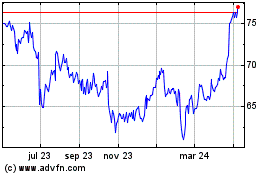
AstraZeneca (NASDAQ:AZN)
Gráfica de Acción Histórica
De Dic 2024 a Ene 2025
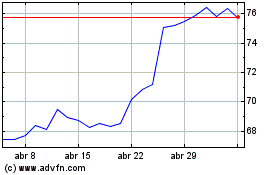
AstraZeneca (NASDAQ:AZN)
Gráfica de Acción Histórica
De Ene 2024 a Ene 2025