- First and only PARP inhibitor plus ARPI combination to
demonstrate statistically significant overall survival (OS) benefit
in patients with metastatic castration-resistant prostate cancer
(mCRPC)
- Results to be shared with global health authorities to
potentially update the TALZENNA label
Pfizer Inc. (NYSE: PFE) today announced positive topline results
from the final prespecified overall survival (OS) analysis of the
TALAPRO-2 study of TALZENNA® (talazoparib), an oral poly ADP-ribose
polymerase (PARP) inhibitor, in combination with XTANDI®
(enzalutamide), an androgen receptor pathway inhibitor (ARPI), in
patients with metastatic castration-resistant prostate cancer
(mCRPC). Results showed a statistically significant and clinically
meaningful improvement in the final OS in all-comers (cohort 1) as
well as in those patients with homologous recombination repair
(HRR) gene-mutated mCRPC (cohort 2), compared to XTANDI alone.
“The TALAPRO-2 results showed that TALZENNA plus XTANDI is the
first and only PARP inhibitor in combination with an ARPI to
significantly improve survival in patients with metastatic
castration-resistant prostate cancer, regardless of mutation
status,” said Roger Dansey, M.D., Chief Development Officer,
Oncology, Pfizer. “Pfizer is dedicated to advancing scientific
breakthroughs in genitourinary cancers, and these exciting
TALAPRO-2 results further highlight our long-standing commitment to
improving survival for men with prostate cancer.”
“These overall survival results indicate potentially
practice-changing efficacy for TALZENNA in combination with XTANDI
for men with metastatic castration-resistant prostate cancer,” said
Neeraj Agarwal, M.D., FASCO, Professor and Presidential Endowed
Chair of Cancer Research at Huntsman Cancer Institute, University
of Utah, and global lead investigator for TALAPRO-2. “Metastatic
castration-resistant prostate cancer is the most advanced and
aggressive stage of the disease, and the TALAPRO-2 results provide
much-needed hope to patients who remain in high unmet need for
effective treatment options.”
At the time of the final analysis, the clinically meaningful
improvement in radiographic progression free survival (rPFS) was
maintained in both cohorts from the prior primary analysis
previously reported and published in The Lancet. In addition, the
safety profile of TALZENNA plus XTANDI was generally consistent
with the known safety profile of each medicine. Detailed results
from TALAPRO-2 will be submitted for presentation at an upcoming
medical congress. These data will also be shared with global health
authorities to potentially support regulatory filings to update and
potentially expand the approved label for TALZENNA.
TALZENNA in combination with XTANDI was approved by the U.S.
Food and Drug Administration (FDA) for the treatment of adult
patients with HRR gene-mutated mCRPC in June 2023. The combination
was also approved by the European Commission in January 2024 for
the treatment of adult patients with mCRPC in whom chemotherapy is
not clinically indicated. TALZENNA is the first and only PARP
inhibitor licensed in the European Union for use with XTANDI for
patients with mCRPC, with or without gene mutations. TALZENNA in
combination with XTANDI is now approved in more than 35 countries
globally for patients with mCRPC.
About Metastatic Castration-Resistant Prostate Cancer
Prostate cancer is the second most common cancer in men and the
fifth most common cause of cancer death among men worldwide, with
an estimated 1.4 million new cases diagnosed in 2022.1 In the U.S.,
it is the most common cancer in men.2 mCRPC is a cancer that has
spread beyond the prostate gland and has progressed despite medical
or surgical treatment to lower testosterone. Approximately 10%–20%
of prostate cancer patients develop mCRPC within 5−7 years of
diagnosis.3 Between 1.2%–2.1% of all prostate cancer cases globally
are mCRPC.4
About TALAPRO-2
The Phase 3 TALAPRO-2 trial is a multicenter, randomized,
double-blind, placebo-controlled study that enrolled 1,035 unique
patients with mCRPC (who had not received new life-prolonging
systemic treatments after documentation of mCRPC) at sites in the
U.S., Canada, Europe, South America, and the Asia-Pacific region.
The study included two patient cohorts: all-comers (n=805, of whom
169 had HRR mutations and 636 did not) and those with HRR gene
mutations (n=399, including 169 patients from Cohort 1 and 230
enrolled in Cohort 2). Patients with castrate testosterone levels
were randomized to receive TALZENNA 0.5 mg/day plus XTANDI
160mg/day, or placebo plus XTANDI 160mg/day.
The primary endpoint of the trial was rPFS, defined as the time
from the date of randomization to first objective evidence of
radiographic progression by blinded independent review, or death,
whichever occurred first, in both Cohort 1 (all-comers) and Cohort
2 (those with HRRm). Secondary endpoints included OS, objective
response rate (ORR), duration of response (DOR), and
prostate-specific antigen (PSA) response.
For more information on the TALAPRO-2 trial (NCT03395197), go to
www.clinicaltrials.gov.
About TALZENNA® (talazoparib)
TALZENNA is an oral inhibitor of poly ADP-ribose polymerase
(PARP), which plays a role in DNA damage repair. Preclinical
studies have demonstrated that TALZENNA blocks PARP enzyme activity
and traps PARP at the site of DNA damage, leading to decreased
cancer cell growth and cancer cell death.
TALZENNA is approved in the U.S., EU, and multiple other regions
for the treatment of adult patients with deleterious or suspected
deleterious gBRCAm HER2-negative locally advanced or metastatic
breast cancer. In the U.S., TALZENNA is approved in combination
with XTANDI for the treatment of adult patients with homologous
recombination repair (HRR) gene-mutated metastatic
castration-resistant prostate cancer (mCRPC). In the EU, TALZENNA
is approved in combination with enzalutamide for the treatment of
adult patients with mCRPC in whom chemotherapy is not clinically
indicated.
TALZENNA® (talazoparib) Indication in the U.S.
TALZENNA is a poly (ADP-ribose) polymerase (PARP) inhibitor
indicated for:
HRR gene-mutated mCRPC:
- In combination with enzalutamide for the treatment of adult
patients with homologous recombination repair (HRR) gene-mutated
metastatic castration-resistant prostate cancer (mCRPC).
Breast Cancer:
- As a single agent, for the treatment of adult patients with
deleterious or suspected deleterious germline BRCA-mutated (gBRCAm)
HER2-negative locally advanced or metastatic breast cancer. Select
patients for therapy based on an FDA-approved companion diagnostic
for TALZENNA.
TALZENNA® (talazoparib) Important Safety
Information
WARNINGS and PRECAUTIONS
Myelodysplastic Syndrome/Acute Myeloid Leukemia
(MDS/AML), including cases with a fatal outcome, has been
reported in patients who received TALZENNA. Overall, MDS/AML has
been reported in 0.4% (3 out of 788) of solid tumor patients
treated with TALZENNA as a single agent in clinical studies. In
TALAPRO-2, MDS/AML occurred in 2 out of 511 (0.4%) patients treated
with TALZENNA and enzalutamide and in 0 out of 517 (0%) patients
treated with placebo and enzalutamide. The durations of TALZENNA
treatment in these five patients prior to developing MDS/AML were
0.3, 1, 2, 3, and 5 years, respectively. Most of these patients had
received previous chemotherapy with platinum agents and/or other
DNA damaging agents including radiotherapy.
Do not start TALZENNA until patients have adequately recovered
from hematological toxicity caused by previous chemotherapy.
Monitor blood counts monthly during treatment with TALZENNA. For
prolonged hematological toxicities, interrupt TALZENNA and monitor
blood counts weekly until recovery. If counts do not recover within
4 weeks, refer the patient to a hematologist for further
investigations including bone marrow analysis and blood sample for
cytogenetics. If MDS/AML is confirmed, discontinue TALZENNA.
Myelosuppression consisting of anemia, neutropenia,
and/or thrombocytopenia have been reported in patients treated with
TALZENNA. In TALAPRO-2, Grade ≥3 anemia, neutropenia, and
thrombocytopenia were reported, respectively, in 45%, 18%, and 8%
of patients receiving TALZENNA and enzalutamide. Overall, 39% of
patients (199/511) required a red blood cell transfusion, including
22% (111/511) who required multiple transfusions. Discontinuation
due to anemia, neutropenia, and thrombocytopenia occurred,
respectively, in 7%, 3%, and 0.4% of patients.
Withhold TALZENNA until patients have adequately recovered from
hematological toxicity caused by previous therapy. Monitor blood
counts monthly during treatment with TALZENNA. If hematological
toxicities do not resolve within 28 days, discontinue TALZENNA and
refer the patient to a hematologist for further investigations
including bone marrow analysis and blood sample for
cytogenetics.
Embryo-Fetal Toxicity TALZENNA can cause fetal harm when
administered to pregnant women. Advise male patients with female
partners of reproductive potential or who are pregnant to use
effective contraception during treatment with TALZENNA and for 4
months after receiving the last dose.
ADVERSE REACTIONS
In TALAPRO-2, serious adverse reactions reported in >2% of
patients included anemia (9%) and fracture (3%). Fatal adverse
reactions occurred in 1.5% of patients, including pneumonia, COVID
infection, and sepsis (1 patient each).
The most common adverse reactions (≥ 10%, all Grades), including
laboratory abnormalities, for patients in the TALAPRO-2 study who
received TALZENNA in combination with enzalutamide vs patients
receiving placebo with enzalutamide were hemoglobin decreased (79%
vs 34%), neutrophils decreased (60% vs 18%), lymphocytes decreased
(58% vs 36%), fatigue (49% vs 40%), platelets decreased (45% vs
8%), calcium decreased (25% vs 11%), nausea (21% vs 17%), decreased
appetite (20% vs 14%), sodium decreased (22% vs 20%), phosphate
decreased (17% vs 13%), fractures (14% vs 10%), magnesium decreased
(14% vs 12%), dizziness (13% vs 9%), bilirubin increased (11% vs
7%), potassium decreased (11% vs 7%), and dysgeusia (10% vs
4.5%).
Clinically relevant adverse reactions in <10% of patients who
received TALZENNA with enzalutamide included abdominal pain (9%),
vomiting (9%), alopecia (7%), dyspepsia (4%), venous
thromboembolism (3%) and stomatitis (2%).
Based on animal studies, TALZENNA may impair fertility in males
of reproductive potential.
DRUG INTERACTIONS
Coadministration with P-gp inhibitors The effect of
coadministration of P-gp inhibitors on talazoparib exposure when
TALZENNA is taken in combination with enzalutamide has not been
studied. Monitor patients for increased adverse reactions and
modify the dosage as recommended for adverse reactions when
TALZENNA is coadministered with a P-gp inhibitor.
Coadministration with BCRP inhibitors Monitor patients
for increased adverse reactions and modify the dosage as
recommended for adverse reactions when TALZENNA is coadministered
with a BCRP inhibitor. Coadministration of TALZENNA with BCRP
inhibitors may increase talazoparib exposure, which may increase
the risk of adverse reactions.
USE IN SPECIFIC POPULATIONS
Renal Impairment The recommended dosage of TALZENNA for
patients with moderate renal impairment (CLcr 30 - 59 mL/min) is
0.35 mg taken orally once daily in combination with enzalutamide.
The recommended dosage of TALZENNA for patients with severe renal
impairment (CLcr 15 - 29 mL/min) is 0.25 mg taken orally once daily
in combination with enzalutamide. No dose adjustment is required
for patients with mild renal impairment. TALZENNA has not been
studied in patients requiring hemodialysis.
Please see full U.S. Prescribing Information and Patient
Information for TALZENNA® (talazoparib) at www.TALZENNA.com.
About XTANDI® (enzalutamide) and Important Safety
Information
XTANDI® (enzalutamide) is an androgen receptor signaling
inhibitor. XTANDI is a standard of care and has received regulatory
approvals in one or more countries around the world for use in men
with metastatic castration-sensitive prostate cancer (mCSPC; also
known as metastatic hormone-sensitive prostate cancer or mHSPC),
metastatic castration-resistant prostate cancer (mCRPC),
non-metastatic castration-resistant prostate cancer (nmCRPC) and
nonmetastatic castration-sensitive prostate cancer (nmCSPC) with
biochemical recurrence at high risk for metastasis (high-risk BCR).
XTANDI is currently approved for one or more of these indications
in more than 90 countries, including in the U.S., EU, and Japan.
Over one million patients have been treated with XTANDI
globally.5
Warnings and Precautions
Seizure occurred in 0.6% of patients receiving XTANDI in
eight randomized clinical trials. In a study of patients with
predisposing factors for seizure, 2.2% of XTANDI-treated patients
experienced a seizure. It is unknown whether anti-epileptic
medications will prevent seizures with XTANDI. Patients in the
study had one or more of the following predisposing factors: use of
medications that may lower the seizure threshold, history of
traumatic brain or head injury, history of cerebrovascular accident
or transient ischemic attack, and Alzheimer’s disease, meningioma,
or leptomeningeal disease from prostate cancer, unexplained loss of
consciousness within the last 12 months, history of seizure,
presence of a space occupying lesion of the brain, history of
arteriovenous malformation, or history of brain infection. Advise
patients of the risk of developing a seizure while taking XTANDI
and of engaging in any activity where sudden loss of consciousness
could cause serious harm to themselves or others. Permanently
discontinue XTANDI in patients who develop a seizure during
treatment.
Posterior Reversible Encephalopathy Syndrome (PRES) There
have been reports of PRES in patients receiving XTANDI. PRES is a
neurological disorder that can present with rapidly evolving
symptoms including seizure, headache, lethargy, confusion,
blindness, and other visual and neurological disturbances, with or
without associated hypertension. A diagnosis of PRES requires
confirmation by brain imaging, preferably MRI. Discontinue XTANDI
in patients who develop PRES.
Hypersensitivity reactions, including edema of the face
(0.5%), tongue (0.1%), or lip (0.1%) have been observed with XTANDI
in eight randomized clinical trials. Pharyngeal edema has been
reported in post-marketing cases. Advise patients who experience
any symptoms of hypersensitivity to temporarily discontinue XTANDI
and promptly seek medical care. Permanently discontinue XTANDI for
serious hypersensitivity reactions.
Ischemic Heart Disease In the combined data of five
randomized, placebo-controlled clinical studies, ischemic heart
disease occurred more commonly in patients on the XTANDI arm
compared to patients on the placebo arm (3.5% vs 2%). Grade 3-4
ischemic events occurred in 1.8% of patients on XTANDI versus 1.1%
on placebo. Ischemic events led to death in 0.4% of patients on
XTANDI compared to 0.1% on placebo. Monitor for signs and symptoms
of ischemic heart disease. Optimize management of cardiovascular
risk factors, such as hypertension, diabetes, or dyslipidemia.
Discontinue XTANDI for Grade 3-4 ischemic heart disease.
Falls and Fractures occurred in patients receiving
XTANDI. Evaluate patients for fracture and fall risk. Monitor and
manage patients at risk for fractures according to established
treatment guidelines and consider use of bone-targeted agents. In
the combined data of five randomized, placebo-controlled clinical
studies, falls occurred in 12% of patients treated with XTANDI
compared to 6% of patients treated with placebo. Fractures occurred
in 13% of patients treated with XTANDI and in 6% of patients
treated with placebo.
Embryo-Fetal Toxicity The safety and efficacy of XTANDI
have not been established in females. XTANDI can cause fetal harm
and loss of pregnancy when administered to a pregnant female.
Advise males with female partners of reproductive potential to use
effective contraception during treatment with XTANDI and for 3
months after the last dose of XTANDI.
Adverse Reactions (ARs) the data from the five randomized
placebo-controlled trials, the most common ARs (≥ 10%) that
occurred more frequently (≥ 2% over placebo) in XTANDI-treated
patients were musculoskeletal pain, fatigue, hot flush,
constipation, decreased appetite, diarrhea, hypertension,
hemorrhage, fall, fracture, and headache. In the
bicalutamide-controlled study, the most common ARs (≥ 10%) reported
in XTANDI-treated patients were asthenia/fatigue, back pain,
musculoskeletal pain, hot flush, hypertension, nausea,
constipation, diarrhea, upper respiratory tract infection, and
weight loss.
In AFFIRM, the placebo-controlled study of metastatic CRPC
(mCRPC) patients who previously received docetaxel, Grade 3 and
higher ARs were reported among 47% of XTANDI-treated patients.
Discontinuations due to ARs were reported for 16% of XTANDI-treated
patients. In PREVAIL, the placebo-controlled study of
chemotherapy-naive mCRPC patients, Grade 3-4 ARs were reported in
44% of XTANDI patients and 37% of placebo patients.
Discontinuations due to ARs were reported for 6% of XTANDI-treated
patients. In TERRAIN, the bicalutamide-controlled study of
chemotherapy-naive mCRPC patients, Grade 3-4 ARs were reported in
39% of XTANDI patients and 38% of bicalutamide patients.
Discontinuations with an AR as the primary reason were reported for
8% of XTANDI patients and 6% of bicalutamide patients.
In PROSPER, the placebo-controlled study of nonmetastatic CRPC
(nmCRPC) patients, Grade 3 or higher ARs were reported in 31% of
XTANDI patients and 23% of placebo patients. Discontinuations with
an AR as the primary reason were reported for 9% of XTANDI patients
and 6% of placebo patients.
In ARCHES, the placebo-controlled study of metastatic CSPC
(mCSPC) patients, Grade 3 or higher ARs were reported in 24% of
XTANDI-treated patients. Permanent discontinuation due to ARs as
the primary reason was reported in 5% of XTANDI patients and 4% of
placebo patients.
In EMBARK, the placebo-controlled study of nonmetastatic CSPC
(nmCSPC) with high-risk biochemical recurrence (BCR) patients,
Grade 3 or higher adverse reactions during the total duration of
treatment were reported in 46% of patients treated with XTANDI plus
leuprolide, 50% of patients receiving XTANDI as a single agent, and
43% of patients receiving placebo plus leuprolide. Permanent
treatment discontinuation due to adverse reactions during the total
duration of treatment as the primary reason was reported in 21% of
patients treated with XTANDI plus leuprolide, 18% of patients
receiving XTANDI as a single agent, and 10% of patients receiving
placebo plus leuprolide.
Lab Abnormalities: Lab abnormalities that occurred in ≥
5% of patients, and more frequently (> 2%) in the XTANDI arm
compared to placebo in the pooled, randomized, placebo-controlled
studies are hemoglobin decrease, neutrophil count decreased, white
blood cell decreased, hyperglycemia, hypermagnesemia, hyponatremia,
hyperphosphatemia, and hypercalcemia.
Hypertension: In the combined data from five randomized
placebo-controlled clinical trials, hypertension was reported in
14.2% of XTANDI patients and 7.4% of placebo patients. Hypertension
led to study discontinuation in < 1% of patients in each
arm.
Drug Interactions
Effect of Other Drugs on XTANDI Avoid coadministration
with strong CYP2C8 inhibitors. If coadministration cannot be
avoided, reduce the dosage of XTANDI.
Avoid coadministration with strong CYP3A4 inducers. If
coadministration cannot be avoided, increase the dosage of
XTANDI.
Effect of XTANDI on Other Drugs Avoid coadministration
with certain CYP3A4, CYP2C9, and CYP2C19 substrates for which
minimal decrease in concentration may lead to therapeutic failure
of the substrate. If coadministration cannot be avoided, increase
the dosage of these substrates in accordance with their Prescribing
Information. In cases where active metabolites are formed, there
may be increased exposure to the active metabolites.
Please access this link for XTANDI’S US Full Prescribing
Information for additional safety information.
About Pfizer Oncology
At Pfizer Oncology, we are at the forefront of a new era in
cancer care. Our industry-leading portfolio and extensive pipeline
includes three core mechanisms of action to attack cancer from
multiple angles, including small molecules, antibody-drug
conjugates (ADCs), and bispecific antibodies, including other
immune-oncology biologics. We are focused on delivering
transformative therapies in some of the world’s most common
cancers, including breast cancer, genitourinary cancer,
hematology-oncology, and thoracic cancers, which includes lung
cancer. Driven by science, we are committed to accelerating
breakthroughs to help people with cancer live better and longer
lives.
About Pfizer: Breakthroughs That Change Patients’
Lives
At Pfizer, we apply science and our global resources to bring
therapies to people that extend and significantly improve their
lives. We strive to set the standard for quality, safety and value
in the discovery, development, and manufacture of health care
products, including innovative medicines and vaccines. Every day,
Pfizer colleagues work across developed and emerging markets to
advance wellness, prevention, treatments, and cures that challenge
the most feared diseases of our time. Consistent with our
responsibility as one of the world’s premier innovative
biopharmaceutical companies, we collaborate with health care
providers, governments, and local communities to support and expand
access to reliable, affordable health care around the world. For
175 years, we have worked to make a difference for all who rely on
us. We routinely post information that may be important to
investors on our website at www.Pfizer.com. In addition, to learn
more, please visit us on www.Pfizer.com and follow us on X at
@Pfizer and @Pfizer News, LinkedIn, YouTube and like us on Facebook
at Facebook.com/Pfizer.
About the Pfizer/Astellas Collaboration
In October 2009, Medivation, Inc., which is now part of Pfizer
(NYSE: PFE), and Astellas (TSE: 4503) entered into a global
agreement to jointly develop and commercialize XTANDI®
(enzalutamide). The companies jointly commercialize XTANDI in the
United States, and Astellas has responsibility for manufacturing
and all additional regulatory filings globally, as well as
commercializing XTANDI outside the United States.
Disclosure Notice
The information contained in this release is as of October 10,
2024. Pfizer assumes no obligation to update forward-looking
statements contained in this release as the result of new
information or future events or developments.
This release contains forward-looking information about Pfizer
Oncology, TALZENNA and XTANDI, including their potential benefits,
the TALAPRO-2 results and plans to share the results with global
health authorities to potentially update the TALZENNA label, that
involves substantial risks and uncertainties that could cause
actual results to differ materially from those expressed or implied
by such statements. Risks and uncertainties include, among other
things, uncertainties regarding the commercial success of TALZENNA
in combination with XTANDI; the uncertainties inherent in research
and development, including the ability to meet anticipated clinical
endpoints, commencement and/or completion dates for our clinical
trials, regulatory submission dates, regulatory approval dates
and/or launch dates, as well as the possibility of unfavorable new
clinical data and further analyses of existing clinical data; the
risk that clinical trial data are subject to differing
interpretations and assessments by regulatory authorities; whether
regulatory authorities will be satisfied with the design of and
results from our clinical studies; whether and when applications
for TALZENNA, XTANDI or a combination may be filed in any
jurisdictions for any potential indications; whether and when any
such applications for TALZENNA, XTANDI or a combination that may be
pending or filed may be approved by regulatory authorities, which
will depend on myriad factors, including making a determination as
to whether the product’s benefits outweigh its known risks and
determination of the product’s efficacy and, if approved, whether
TALZENNA, XTANDI or a combination will be commercially successful;
decisions by regulatory authorities impacting labeling,
manufacturing processes, safety and/or other matters that could
affect the availability or commercial potential of TALZENNA, XTANDI
or a combination; uncertainties regarding the impact of COVID-19 on
Pfizer’s business, operations and financial results; and
competitive developments.
A further description of risks and uncertainties can be found in
Pfizer’s Annual Report on Form 10-K for the fiscal year ended
December 31, 2023, and in its subsequent reports on Form 10-Q,
including in the sections thereof captioned “Risk Factors” and
“Forward-Looking Information and Factors That May Affect Future
Results”, as well as in its subsequent reports on Form 8-K, all of
which are filed with the U.S. Securities and Exchange Commission
and available at www.sec.gov and www.pfizer.com.
References
1 Bray F, Laversanne M, Sung H, et al. Global cancer statistics
2022: GLOBOCAN estimates of incidence and mortality worldwide for
36 cancers in 185 countries. CA: A Cancer Journal for Clinicians.
2024;74(3):229-263. Published 2024 April 4. doi:10.3322/caac.21834
2 American Cancer Society. Key Statistics for Prostate Cancer.
Accessed August 2024. *other than non-melanoma skin cancer 3 Kirby
M, Hirst C, Crawford ED. Characterising the castration-resistant
prostate cancer population: a systematic review. Int J Clin Pract.
2011 Nov;65(11):1180-92. doi: 10.1111/j.1742-1241.2011.02799.x.
PMID: 21995694. 4 Shore N, Oliver L, Shui I, Gayle A, Wong OY, Kim
J, Payne S, Amin S, Ghate S. Systematic Literature Review of the
Epidemiology of Advanced Prostate Cancer and Associated Homologous
Recombination Repair Gene Alterations. J Urol. 2021
Apr;205(4):977-986. doi: 10.1097/JU.0000000000001570. Epub 2020 Dec
17. PMID: 33332152.
https://www.auajournals.org/doi/10.1097/JU.0000000000001570 5 Data
on file. Northbrook, IL: Astellas Inc.
View source
version on businesswire.com: https://www.businesswire.com/news/home/20241009804174/en/
Media Contact: +1 (212) 733-1226 PfizerMediaRelations@Pfizer.com
Investor Contact: +1 (212) 733-4848 IR@Pfizer.com
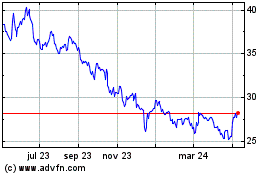
Pfizer (NYSE:PFE)
Gráfica de Acción Histórica
De Oct 2024 a Nov 2024
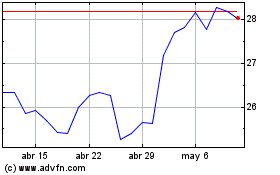
Pfizer (NYSE:PFE)
Gráfica de Acción Histórica
De Nov 2023 a Nov 2024