– ZUMA-5 Analysis Shows Median
Progression-Free Survival of 62.2 Months and Median Duration of
Response of 60.4 Months After Median Follow-Up of More Than Five
Years –
– Over Half of Patients Alive at Time of
Analysis, with No Need for Subsequent Therapy and Rare Instances of
Late Disease Progression, Indicating Curative Potential –
Kite, a Gilead Company (Nasdaq: GILD), today announced results
from a five-year follow-up analysis of ZUMA-5, a Phase 2 study of
Yescarta® (axicabtagene ciloleucel) in patients with
relapsed/refractory non-Hodgkin lymphomas (NHL) including
follicular lymphoma (FL) or marginal zone lymphoma (MZL). The
analysis demonstrated that after a median follow-up of more than
five years, patients treated with Yescarta continued to experience
durable response and long-term survival. The data were shared in an
oral presentation (Abstract #864) during the 66th American Society
of Hematology (ASH) Annual Meeting and Exposition.
“Relapsed or refractory non-Hodgkin lymphomas, including
follicular lymphoma and marginal zone lymphoma, are generally
considered to be incurable, with most patients ultimately
relapsing,” said Dr. Sattva S. Neelapu, lead investigator, The
University of Texas MD Anderson Cancer Center. “These impressive
results demonstrate the continued durable clinical benefit and
manageable long-term safety profile of axi-cel and give us hope
that it may have a curative effect on these difficult-to-treat
blood cancers.”
In ZUMA-5, 159 patients were enrolled (127 FL, 31 MZL, 1 DLBCL
[later excluded]). At a median follow-up of 64.6 months (range,
32.3-81.4; FL: 65.7, MZL: 55.8), the overall response rate (ORR)
was 90% and the complete response (CR) was 75%. Among patients who
achieved a CR, 58% remained in CR at the time of data cutoff. The
median duration of response (DOR) was 60.4 months (95% CI, 39.7-not
estimable [NE]; FL: 60.4, MZL: not reached [NR]), with estimated
60-month DOR of 53.4% (95% CI, 43.9-62.0; FL: 52.2%, MZL:
60.0%).
Median progression-free survival (PFS) was 62.2 months (95% CI,
34.9-NE; FL: 57.3, MZL: NR). PFS rates at 60 months in patients
with FL were consistent regardless of high-risk
characteristics.
Median time to next therapy was NR in all patients with NHL (95%
CI, 38.6-NE; consistent by disease type), with a 60-month estimated
rate of 53.3% (95% CI, 45.0-60.9; FL: 54.0%, MZL: 50.9%). At data
cutoff, 55% of patients (n=87) were alive with no new anticancer
therapy. The median overall survival (OS) was NR (95% CI, NE-NE;
consistent by disease type), and the 60-month OS estimate was 69.0%
(95% CI, 60.8-75.8; FL: 68.9, MZL: 71.1).
“There is growing evidence that people with follicular lymphoma
and marginal zone lymphoma can experience long-term survival after
one Yescarta treatment,” said Dominique Tonelli, VP, Global Head of
Medical Affairs, Kite. “With no lymphoma-specific events in the
five-year follow-up of ZUMA-5 patients, Yescarta may offer patients
the chance to live longer without need for subsequent therapy and a
potential cure.”
No new Yescarta-related safety signals emerged in the five-year
analysis. One patient progressed after the data cutoff of the
four-year analysis and no patients died of disease progression
after the prior analysis. Among treated patients (n=152, 124 FL, 28
MZL), three new events not related to Yescarta were reported after
the four-year analysis, including Grade 3 metastasis, Grade 1
bladder cancer, and Grade 4 myelodysplastic syndrome (a serious
adverse event). One patient died of pneumonia, unrelated to
Yescarta. At any time on trial, a total of 46 patients died, due to
progressive disease (n=14), secondary malignancies (n=6),
infections (n=11), or another or unknown cause (n=15).
About ZUMA-5
ZUMA-5 is a single-arm, open-label, international, multicenter
Phase 2 study evaluating 159 adult patients with R/R NHL (FL and
MZL) who received at least two prior lines of systemic therapy,
including the combination of an anti-CD20 monoclonal antibody and
an alkylating agent. The primary endpoint was ORR, and secondary
endpoints included CR rate, ORR and CR in patients who had received
three or more lines of prior therapy, DOR, OS, PFS and incidence of
adverse events.
About NHL
FL and MZL are both forms of indolent NHL in which malignant
tumors slowly grow but can become more aggressive over time.
FL is the most common form of indolent lymphoma and the second
most common type of lymphoma globally. It accounts for
approximately 22 percent of all lymphomas diagnosed worldwide. MZL
is the third most common lymphoma, accounting for 8 to 12 percent
of all B-cell NHLs.
Despite advances in management and substantial improvements in
long-term survival, patients living with FL have varied outcomes.
Currently, there are limited options for the treatment of relapsed
or refractory FL and MZL after two or more lines of therapy.
About Yescarta
Please see full Prescribing Information, including BOXED
WARNING and Medication Guide.
YESCARTA is a CD19-directed genetically modified autologous T
cell immunotherapy indicated for the treatment of:
- Adult patients with large B-cell lymphoma that is refractory to
first-line chemoimmunotherapy or that relapses within 12 months of
first-line chemoimmunotherapy.
- Adult patients with relapsed or refractory large B-cell
lymphoma after two or more lines of systemic therapy, including
diffuse large B-cell lymphoma (DLBCL) not otherwise specified,
primary mediastinal large B-cell lymphoma, high grade B-cell
lymphoma, and DLBCL arising from follicular lymphoma. Limitations
of Use: YESCARTA is not indicated for the treatment of patients
with primary central nervous system lymphoma.
- Adult patients with relapsed or refractory follicular lymphoma
(FL) after two or more lines of systemic therapy. This indication
is approved under accelerated approval based on response rate.
Continued approval for this indication may be contingent upon
verification and description of clinical benefit in confirmatory
trial(s).
U.S. IMPORTANT SAFETY INFORMATION
BOXED WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC
TOXICITIES and SECONDARY HEMATOLOGICAL MALIGNANCIES
- Cytokine Release Syndrome (CRS), including fatal or
life-threatening reactions, occurred in patients receiving
YESCARTA. Do not administer YESCARTA to patients with active
infection or inflammatory disorders. Treat severe or
life-threatening CRS with tocilizumab or tocilizumab and
corticosteroids.
- Neurologic toxicities, including fatal or life-threatening
reactions, occurred in patients receiving YESCARTA, including
concurrently with CRS or after CRS resolution. Monitor for
neurologic toxicities after treatment with YESCARTA. Provide
supportive care and/or corticosteroids, as needed.
- T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies, including
YESCARTA.
- YESCARTA is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
YESCARTA and TECARTUS REMS Program.
CYTOKINE RELEASE SYNDROME (CRS)
CRS, including fatal or life-threatening reactions, occurred
following treatment with YESCARTA. CRS occurred in 90% (379/422) of
patients with non-Hodgkin lymphoma (NHL) receiving YESCARTA,
including ≥ Grade 3 (Lee grading system1) CRS in 9%. CRS occurred
in 93% (256/276) of patients with large B-cell lymphoma (LBCL),
including ≥ Grade 3 CRS in 9%. Among patients with LBCL who died
after receiving YESCARTA, four had ongoing CRS events at the time
of death. For patients with LBCL in ZUMA-1, the median time to
onset of CRS was 2 days following infusion (range: 1 to 12 days)
and the median duration of CRS was 7 days (range: 2 to 58 days).
For patients with LBCL in ZUMA-7, the median time to onset of CRS
was 3 days following infusion (range: 1 to 10 days) and the median
duration was 7 days (range: 2 to 43 days).
CRS occurred in 84% (123/146) of patients with indolent
non-Hodgkin lymphoma (iNHL) in ZUMA-5, including ≥ Grade 3 CRS in
8%. Among patients with iNHL who died after receiving YESCARTA, one
patient had an ongoing CRS event at the time of death. The median
time to onset of CRS was 4 days (range: 1 to 20 days) and the
median duration was 6 days (range: 1 to 27 days) for patients with
iNHL.
Key manifestations of CRS (≥ 10%) in all patients combined
included fever (85%), hypotension (40%), tachycardia (32%), chills
(22%), hypoxia (20%), headache (15%), and fatigue (12%). Serious
events that may be associated with CRS include, cardiac arrhythmias
(including atrial fibrillation and ventricular tachycardia), renal
insufficiency, cardiac failure, respiratory failure, cardiac
arrest, capillary leak syndrome, multi-organ failure, and
hemophagocytic lymphohistiocytosis/macrophage activation syndrome
(HLH/MAS).
The impact of tocilizumab and/or corticosteroids on the
incidence and severity of CRS was assessed in two subsequent
cohorts of LBCL patients in ZUMA-1. Among patients who received
tocilizumab and/or corticosteroids for ongoing Grade 1 events. CRS
occurred in 93% (38/41), including 2% (1/41) with Grade 3 CRS; no
patients experienced a Grade 4 or 5 event. The median time to onset
of CRS was 2 days (range: 1 to 8 days) and the median duration of
CRS was 7 days (range: 2 to 16 days).
Prophylactic treatment with corticosteroids was administered to
a cohort of 39 patients for 3 days beginning on the day of infusion
of YESCARTA. Thirty-one of the 39 patients (79%) developed CRS at
which point the patients were managed with tocilizumab and/or
therapeutic doses of corticosteroids with no patients developing
Grade 3 or higher CRS. The median time to onset of CRS was 5 days
(range: 1 to 15 days) and the median duration of CRS was 4 days
(range: 1 to 10 days). Although there is no known mechanistic
explanation, consider the risk and benefits of prophylactic
corticosteroids in the context of pre-existing comorbidities for
the individual patient and the potential for the risk of Grade 4
and prolonged neurologic toxicities.
Ensure that 2 doses of tocilizumab are available prior to
infusion of YESCARTA. Monitor patients at least daily for 7 days at
the certified healthcare facility following infusion for signs and
symptoms of CRS. Monitor patients for signs or symptoms of CRS for
4 weeks after infusion. Counsel patients to seek immediate medical
attention should signs or symptoms of CRS occur at any time. At the
first sign of CRS, institute treatment with supportive care,
tocilizumab, or tocilizumab and corticosteroids as indicated.
NEUROLOGIC TOXICITIES
Neurologic toxicities (including immune effector cell-associated
neurotoxicity syndrome) that were fatal or life- threatening
occurred. Neurologic toxicities occurred in 78% (330/422) of all
patients with NHL receiving YESCARTA, including ≥ Grade 3 in 25%.
Neurologic toxicities occurred in 87% (94/108) of patients with
LBCL in ZUMA-1, including ≥ Grade 3 in 31% and in 74% (124/168) of
patients in ZUMA-7 including ≥ Grade 3 in 25%. The median time to
onset was 4 days (range: 1-43 days) and the median duration was 17
days for patients with LBCL in ZUMA-1. The median time to onset for
neurologic toxicity was 5 days (range:1- 133 days) and median
duration was 15 days in patients with LBCL in ZUMA-7. Neurologic
toxicities occurred in 77% (112/146) of patients with iNHL,
including ≥ Grade 3 in 21%. The median time to onset was 6 days
(range: 1-79 days) and the median duration was 16 days.
Ninety-eight percent of all neurologic toxicities in patients with
LBCL and 99% of all neurologic toxicities in patients with iNHL
occurred within the first 8 weeks of YESCARTA infusion. Neurologic
toxicities occurred within the first 7 days of infusion for 87% of
affected patients with LBCL and 74% of affected patients with
iNHL.
The most common neurologic toxicities (≥ 10%) in all patients
combined included encephalopathy (50%), headache (43%), tremor
(29%), dizziness (21%), aphasia (17%), delirium (15%), and insomnia
(10%). Prolonged encephalopathy lasting up to 173 days was noted.
Serious events, including aphasia, leukoencephalopathy, dysarthria,
lethargy, and seizures occurred. Fatal and serious cases of
cerebral edema and encephalopathy, including late-onset
encephalopathy, have occurred.
The impact of tocilizumab and/or corticosteroids on the
incidence and severity of neurologic toxicities was assessed in 2
subsequent cohorts of LBCL patients in ZUMA-1. Among patients who
received corticosteroids at the onset of Grade 1 toxicities,
neurologic toxicities occurred in 78% (32/41) and 20% (8/41) had
Grade 3 neurologic toxicities; no patients experienced a Grade 4 or
5 event. The median time to onset of neurologic toxicities was 6
days (range: 1-93 days) with a median duration of 8 days (range:
1-144 days). Prophylactic treatment with corticosteroids was
administered to a cohort of 39 patients for 3 days beginning on the
day of infusion of YESCARTA. Of those patients, 85% (33/39)
developed neurologic toxicities, 8% (3/39) developed Grade 3, and
5% (2/39) developed Grade 4 neurologic toxicities. The median time
to onset of neurologic toxicities was 6 days (range: 1-274 days)
with a median duration of 12 days (range: 1-107 days). Prophylactic
corticosteroids for management of CRS and neurologic toxicities may
result in higher grade of neurologic toxicities or prolongation of
neurologic toxicities, delay the onset and decrease the duration of
CRS.
Monitor patients for signs and symptoms of neurologic toxicities
at least daily for 7 days at the certified healthcare facility, and
for 4 weeks thereafter, and treat promptly.
REMS
Because of the risk of CRS and neurologic toxicities, YESCARTA
is available only through a restricted program called the YESCARTA
and TECARTUS REMS Program which requires that: Healthcare
facilities that dispense and administer YESCARTA must be enrolled
and comply with the REMS requirements and must have on-site,
immediate access to a minimum of 2 doses of tocilizumab for each
patient for infusion within 2 hours after YESCARTA infusion, if
needed for treatment of CRS. Certified healthcare facilities must
ensure that healthcare providers who prescribe, dispense, or
administer YESCARTA are trained about the management of CRS and
neurologic toxicities. Further information is available at
www.YescartaTecartusREMS.com or 1-844-454-KITE (5483).
HYPERSENSITIVITY REACTIONS
Allergic reactions, including serious hypersensitivity reactions
or anaphylaxis, may occur with the infusion of YESCARTA.
SERIOUS INFECTIONS
Severe or life-threatening infections occurred. Infections (all
grades) occurred in 45% of patients with NHL. Grade 3 or higher
infections occurred in 17% of patients, including ≥ Grade 3 or
higher infections with an unspecified pathogen in 12%, bacterial
infections in 5%, viral infections in 3%, and fungal infections in
1%. YESCARTA should not be administered to patients with clinically
significant active systemic infections. Monitor patients for signs
and symptoms of infection before and after infusion and treat
appropriately. Administer prophylactic antimicrobials according to
local guidelines.
Febrile neutropenia was observed in 36% of all patients with NHL
and may be concurrent with CRS. In the event of febrile
neutropenia, evaluate for infection and manage with broad-spectrum
antibiotics, fluids, and other supportive care as medically
indicated.
In immunosuppressed patients, including those who have received
YESCARTA, life-threatening and fatal opportunistic infections
including disseminated fungal infections (e.g., candida sepsis and
aspergillus infections) and viral reactivation (e.g., human herpes
virus-6 [HHV-6] encephalitis and JC virus progressive multifocal
leukoencephalopathy [PML]) have been reported. The possibility of
HHV-6 encephalitis and PML should be considered in immunosuppressed
patients with neurologic events and appropriate diagnostic
evaluations should be performed. Hepatitis B virus (HBV)
reactivation, in some cases resulting in fulminant hepatitis,
hepatic failure, and death, can occur in patients treated with
drugs directed against B cells, including YESCARTA. Perform
screening for HBV, HCV, and HIV in accordance with clinical
guidelines before collection of cells for manufacturing.
PROLONGED CYTOPENIAS
Patients may exhibit cytopenias for several weeks following
lymphodepleting chemotherapy and YESCARTA infusion. ≥ Grade 3
cytopenias not resolved by Day 30 following YESCARTA infusion
occurred in 39% of all patients with NHL and included neutropenia
(33%), thrombocytopenia (13%), and anemia (8%). Monitor blood
counts after infusion.
HYPOGAMMAGLOBULINEMIA
B-cell aplasia and hypogammaglobulinemia can occur.
Hypogammaglobulinemia was reported as an adverse reaction in 14% of
all patients with NHL. Monitor immunoglobulin levels after
treatment and manage using infection precautions, antibiotic
prophylaxis, and immunoglobulin replacement. The safety of
immunization with live viral vaccines during or following YESCARTA
treatment has not been studied. Vaccination with live virus
vaccines is not recommended for at least 6 weeks prior to the start
of lymphodepleting chemotherapy, during YESCARTA treatment, and
until immune recovery following treatment.
SECONDARY MALIGNANCIES
Patients treated with YESCARTA may develop secondary
malignancies. T cell malignancies have occurred following treatment
of hematologic malignancies with BCMA- and CD19-directed
genetically modified autologous T cell immunotherapies, including
YESCARTA. Mature T cell malignancies, including CAR-positive
tumors, may present as soon as weeks following infusion, and may
include fatal outcomes.
Monitor life-long for secondary malignancies. In the event that
a secondary malignancy occurs, contact Kite at 1-844-454-KITE
(5483) to obtain instructions on patient samples to collect for
testing.
EFFECTS ON ABILITY TO DRIVE AND USE MACHINES
Due to the potential for neurologic events, including altered
mental status or seizures, patients are at risk for altered or
decreased consciousness or coordination in the 8 weeks following
YESCARTA infusion. Advise patients to refrain from driving and
engaging in hazardous occupations or activities, such as operating
heavy or potentially dangerous machinery, during this initial
period.
ADVERSE REACTIONS
The most common non-laboratory adverse reactions (incidence ≥
20%) in patients with LBCL in ZUMA-7 included fever, CRS, fatigue,
hypotension, encephalopathy, tachycardia, diarrhea, headache,
musculoskeletal pain, nausea, febrile neutropenia, chills, cough,
infection with unspecified pathogen, dizziness, tremor, decreased
appetite, edema, hypoxia, abdominal pain, aphasia, constipation,
and vomiting.
The most common adverse reactions (incidence ≥ 20%) in patients
with LBCL in ZUMA-1 included CRS, fever, hypotension,
encephalopathy, tachycardia, fatigue, headache, decreased appetite,
chills, diarrhea, febrile neutropenia, infections with pathogen
unspecified, nausea, hypoxia, tremor, cough, vomiting, dizziness,
constipation, and cardiac arrhythmias.
The most common non-laboratory adverse reactions (incidence ≥
20%) in patients with iNHL in ZUMA-5 included fever, CRS,
hypotension, encephalopathy, fatigue, headache, infections with
pathogen unspecified, tachycardia, febrile neutropenia,
musculoskeletal pain, nausea, tremor, chills, diarrhea,
constipation, decreased appetite, cough, vomiting, hypoxia,
arrhythmia, and dizziness.
About Kite
Kite, a Gilead Company, is a global biopharmaceutical company
based in Santa Monica, California, focused on achieving cures with
cell therapy. As the global cell therapy leader, Kite has treated
more patients with CAR T-cell therapy than any other company. Kite
has the largest in-house cell therapy manufacturing network in the
world, spanning process development, vector manufacturing, clinical
trial supply and commercial product manufacturing. For more
information on Kite, please visit www.kitepharma.com.
About Gilead Sciences
Gilead Sciences, Inc. is a biopharmaceutical company that has
pursued and achieved breakthroughs in medicine for more than three
decades, with the goal of creating a healthier world for all
people. The company is committed to advancing innovative medicines
to prevent and treat life-threatening diseases, including HIV,
viral hepatitis, COVID-19, cancer, and inflammation. Gilead
operates in more than 35 countries worldwide, with headquarters in
Foster City, Calif. Gilead acquired Kite in 2017.
Forward-Looking
Statements
This press release includes forward-looking statements, within
the meaning of the Private Securities Litigation Reform Act of 1995
that are subject to risks, uncertainties and other factors,
including the ability of Gilead and Kite to initiate, progress or
complete clinical trials within currently anticipated timelines or
at all, and the possibility of unfavorable results from ongoing or
additional clinical studies, including those involving Yescarta
(such as ZUMA-5); uncertainties relating to regulatory applications
and related filing and approval timelines, including pending or
potential applications for indications currently under evaluation;
and any assumptions underlying any of the foregoing. These and
other risks, uncertainties and other factors are described in
detail in Gilead’s Quarterly Report on Form 10-Q for the quarter
ended September 30, 2024, as filed with the U.S. Securities and
Exchange Commission. These risks, uncertainties and other factors
could cause actual results to differ materially from those referred
to in the forward-looking statements. All statements other than
statements of historical fact are statements that could be deemed
forward-looking statements. The reader is cautioned that any such
forward-looking statements are not guarantees of future performance
and involve risks and uncertainties and is cautioned not to place
undue reliance on these forward-looking statements. All
forward-looking statements are based on information currently
available to Gilead and Kite, and Gilead and Kite assume no
obligation and disclaim any intent to update any such
forward-looking statements.
Yescarta, Gilead, the Gilead logo, Kite, the
Kite logo are trademarks of Gilead Sciences, Inc., or its related
companies.
For more information on Kite, please visit the
company’s website at www.kitepharma.com. Follow Kite on social
media on X (@KitePharma) and LinkedIn.
View source
version on businesswire.com: https://www.businesswire.com/news/home/20241209207499/en/
Blair Baumwell, Gilead Media public_affairs@gilead.com
Jacquie Ross, Investors investor_relations@gilead.com
Gilead Sciences (NASDAQ:GILD)
Gráfica de Acción Histórica
De Nov 2024 a Dic 2024
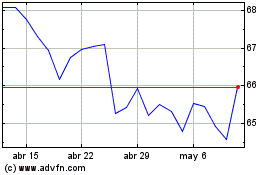
Gilead Sciences (NASDAQ:GILD)
Gráfica de Acción Histórica
De Dic 2023 a Dic 2024
