Coral Gables, FL, March 3, 2024. MSP Recovery, Inc. d/b/a
LifeWallet (NASDAQ: LIFW) (“LifeWallet” or “the Company”) announces
a comprehensive settlement with 28 affiliated property and casualty
insurers (“P&C Insurers”) that, in addition to settling
existing claims, establishes a going-forward process to
collaboratively and timely resolve future claims, as well as share
important historical data that is expected to enhance LifeWallet’s
claims reconciliation capabilities, benefiting its Medicare clients
across the mainland U.S. and Puerto Rico. The settlement includes:
- The P&C Insurers’ agreement to
provide ten years of historical data (identifying all claims
processed from January 1, 2014, through the present) and data
sharing of future claims, extending out for one year, assisting
LifeWallet in reconciling its current and future assigned Medicare
claims;
- The P&C Insurers’
Implementation of LifeWallet’s coordination of benefits
clearinghouse solution;
- A 5-year agreement to resolve
cooperatively, or through binding mediation, relevant Medicare
claims (liens) that LifeWallet owns today and in the future;
- The P&C Insurers’ agreement
that they are primary payers for any unreimbursed Medicare lien
that LifeWallet identifies from data sharing, and the P&C
Insurers’ agreement to assign all rights to collect against other
third parties that either failed to pay liens or collected twice
from Medicare funds and the P&C Insurers; and
- A cash payment from the P&C
Insurers to LifeWallet to settle existing historical claims (amount
subject to confidentiality).
Settlement Significance
This settlement agreement is the result of
LifeWallet’s more than ten-year commitment to revolutionize the
fragmented healthcare reimbursement system with data-driven
solutions, utilizing its extensive legal infrastructure to enforce
Primary Payer1 obligations (from mostly property and casualty
insurers), through years of federal and state litigation. The
settlement creates an environment where Secondary Payers,2 such as
health insurance plans and healthcare providers, discover Medicare
liens owed to them and recover conditional payments from
responsible primary plans, such as property and casualty insurers.
As described by a federal appellate judge, when Secondary Payers
“recover efficiently from Primary Payers, the Medicare Trust Fund
does achieve cost savings.”3
LifeWallet is of the opinion the settlement
demonstrates proof of concept that can potentially be replicated
with other Primary Payers. However, LifeWallet notes that this
settlement is not a guarantee that LifeWallet’s portfolio of
assigned claims (owed by other Primary Payers) can be settled with
the same or similar terms. The settlement value is a combination of
monetary and non-monetary considerations, with the non-monetary
considerations involving LifeWallet obtaining data on all the
claims that were processed and paid by the P&C Insurers, and
the P&C Insurers’ assignment of rights to collect against other
responsible parties. This will enhance LifeWallet’s ability to
discover liens and recover payments owed, more quickly than through
litigation. It also enables LifeWallet to pursue a diversified
number of entities that failed to pay liens or collected twice for
the same bills, both from the insurer and LifeWallet’s assignor
clients.
LifeWallet Founder and CEO, John H. Ruiz,
commented, “Today’s news shows LifeWallet’s significant progress in
implementing our business model and commitment to achieving
positive outcomes for healthcare entities across the country.”
LifeWallet Co-Founder and Chief Legal Officer, Frank C. Quesada,
added, “We are hopeful these collaborative efforts will pave the
way for similar resolutions with other property and casualty
insurers, including those currently in negotiations with
LifeWallet. This benefits all stakeholders willing to work together
to address issues that have plagued the healthcare industry for
decades and be part of the solution to improve the healthcare
system for insurers, providers, and patients alike.”
________________________1 Primary Plans” or
“Primary Payers,” when used in the Medicare Secondary Payer
context, means “any entity that is or was required or responsible
to make payment with respect to an item
or service (or any portion thereof) under a primary
plan. These entities include, but are not limited to, insurers or
self-insurers, third party administrators, and all employers that
sponsor or contribute to group health plans or large
group health plans.” 42 C.F.R. § 411.21.2 “Secondary Payers”
includes Medicare Part C plans, as well as downstream entities. MSP
Recovery Claims, Series LLC v. ACE Am. Ins. Co., 974 F.3d 1305,
1316 (11th Cir. 2020).3 In re Avandia Mktg., Sales Pracs. &
Prod. Liab. Litig., 685 F.3d 353, 365 (3d Cir. 2012).
Solving An Industry Problem
The failure to follow the Medicare Secondary
Payer Act (“MSP Act”) is costing taxpayers billions of dollars. The
law serves to protect original Medicare, Medicare Advantage plans,
and downstream entities. Medicare loses money because it “pays in
the dark” and relies on Primary Payers to report information to
Centers for Medicare & Medicaid Services (“CMS”).4 Primary
Payers, however, often do not have the tools and resources in place
to identify every reportable event. LifeWallet’s data matching
initiatives have created transparency, enabling LifeWallet’s
Secondary Payer clients to discover when a Medicare beneficiary is
insured through other sources and recover reimbursements.
Historical
reconciliation, assignment of P&C Insurers’ rights, and 5-year
agreement to resolve unreimbursed Medicare liens, without the need
for litigation
This settlement is a
crucial step in addressing the systemic problems arising from
incomplete reporting because the settlement requires the P&C
Insurers to share ten years of historical data on first and
third-party claims. The P&C Insurers have agreed that for each
unreimbursed Medicare lien that LifeWallet identifies from the
historical data, they will assign to LifeWallet any rights they
have to collect against those third parties that either failed to
pay liens or collected twice from LifeWallet’s clients (that paid
with Medicare funds) and the P&C Insurer. This process further
enhances LifeWallet’s ability to discover liens owed by P&C
Insurers and any other third parties that had payment
responsibility, and to collect on its portfolio of current claim
rights.
Furthermore, the
settlement sets up a five-year agreement whereby the P&C
Insurers agree to either resolve cooperatively, or through binding
mediation, any future rights to unreimbursed liens, providing a
structured process to work through lien repayment on a timely
basis, without the need for costly and inefficient litigation. This
applies to current and future LifeWallet clients.
Working
towards real-time payer-based identification through LifeWallet’s
coordination of benefits clearinghouse
Utilizing
LifeWallet’s unique payer-based knowledge, artificial intelligence
(“AI”) and blockchain-based LifeChain integrations, LifeWallet has
developed a comprehensive coordination of benefits clearinghouse.
This builds upon the Company’s previously announced initiatives:
“MSP Recovery and Palantir to Transform Connectivity Across the
U.S. Healthcare System” and “LifeWallet Announces Significant
Enhancements to LifeWallet Health with Advanced Tools for Providers
and Patients.”5 Through the seamless convergence of information
technology and direct Application Programming Interface (“API”)
and/or similar data transfer protocols, LifeWallet’s clients and
Primary Payers can efficiently coordinate benefits. This integrated
offering creates transparency and efficiency in claims
reconciliation. Traditional methods that rely on Primary Payers to
report to Medicare are flawed because Primary Payers often lack the
necessary tools, resources, and data points to comply with the
stringent data field requirements imposed by CMS. A direct data
connection allows for more efficient communication of payments and
coordination of recovery efforts when conditional payments are
made.
This technology
creates a substantial advancement in benefits management,
coordination of insurance coverage, and claims resolution between
parties. LifeWallet’s ability to identify and coordinate benefits
for medical claims will give its clients a significant payment
reconciliation advantage over the rest of the industry. This also
allows patients to gain access (with proper security protocols) to
their claims data, which will provide clarity into what was billed,
who originated the bill, and which payer(s) made payment(s). David
Simmons, who has held several MSP policy roles at CMS and founded
healthcare consulting firm, Ten One Strategies, commented on the
LifeWallet coordination of benefits clearinghouse, saying, “Having
all parties coordinate early in the process demonstrates that payer
coordination can be an efficient and proactive partnership.”
________________________4 United States v.
Baxter Int’l, Inc., 345 F.3d 866, 901 (11th Cir. 2003) (“When
Medicare pays, therefore, it is paying ‘in the dark’—it does not
know, and cannot know, whether someone else will pay.).5 October
11, 2021 Press Release re: MSP Recovery, now LifeWallet (NASDAQ:
LIFW) and Palantir Technologies Inc., April 5, 2023 Press Release
re: LifeWallet (NASDAQ: LIFW)
LifeWallet’s Business Model
Since its founding in 2014 as MSP Recovery,
LifeWallet has aimed to disrupt the antiquated healthcare
reimbursement system with data-driven solutions, utilizing advanced
technology and extensive legal expertise to recover reimbursements
for Medicare, Medicaid, and commercial entities.
LifeWallet Founder and CEO, John H. Ruiz, who
worked with LifeWallet’s counsel, Charlie Whorton, to achieve this
settlement resolution, said, “This settlement encompasses the two
most important concepts that LifeWallet set out to resolve —
discover conditional payments and recover reimbursement from
primary payers. While some insurers have failed to follow the law
and been uncooperative, we commend those insurers that have stepped
up to the plate to do what is required.” Ruiz continued, “Our goal
has been to create a more compliant and transparent environment,
where secondary payers and primary plans are coordinating and
sharing information. Such an environment ultimately serves to
preserve the Medicare Trust Funds.”
Forward Looking Statements
This press release contains forward-looking
statements within the meaning of the federal securities laws.
Forward-looking statements may generally be identified by the use
of words such as “anticipate,” “believe,” “expect,” “intend,”
“plan" and “will” or, in each case, their negative, or other
variations or comparable terminology. These forward-looking
statements include all matters that are not historical facts,
including for example statements regarding potential future
settlements. By their nature, forward-looking statements involve
risks and uncertainties because they relate to events and depend on
circumstances that may or may not occur in the future. As a result,
these statements are not guarantees of future performance or
results and actual events may differ materially from those
expressed in or suggested by the forward-looking statements. Any
forward-looking statement made by the Company herein speaks only as
of the date made. New risks and uncertainties come up from time to
time, and it is impossible for the Company to predict or identify
all such events or how they may affect it. the Company has no
obligation, and does not intend, to update any forward-looking
statements after the date hereof, except as required by federal
securities laws. Factors that could cause these differences
include, but are not limited to, the Company’s ability to
capitalize on its assignment agreements and recover monies that
were paid by the assignors; the inherent uncertainty surrounding
settlement negotiations and/or litigation, including with respect
to both the amount and timing of any such results; the success of
the Company's scheduled settlement mediations; the validity of the
assignments of claims to the Company; negative publicity concerning
healthcare data analytics and payment accuracy; and those other
factors included in the Company’s Annual Report on Form 10-K,
Quarterly Reports on Form 10-Q and other reports filed by it with
the SEC. These statements constitute the Company’s cautionary
statements under the Private Securities Litigation Reform Act of
1995.
About LifeWallet
Founded in 2014 as MSP Recovery, LifeWallet has
become a Medicare, Medicaid, commercial, and secondary payer
reimbursement recovery leader, disrupting the antiquated healthcare
reimbursement system with data-driven solutions to secure
recoveries from responsible parties. LifeWallet provides
comprehensive solutions for multiple industries including
healthcare, legal, education, and sports NIL, while innovating
technologies to help save lives. For more information, visit:
LIFEWALLET.COM
Contact
Media:
ICR, Inc.
lifewallet@icrinc.com
Investors:
Investors@LifeWallet.com
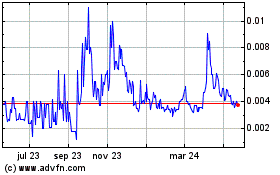
MSP Recovery (NASDAQ:LIFWW)
Gráfica de Acción Histórica
De Nov 2024 a Dic 2024
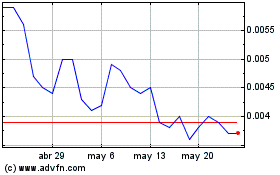
MSP Recovery (NASDAQ:LIFWW)
Gráfica de Acción Histórica
De Dic 2023 a Dic 2024