Final results from the DAYBREAK long-term
extension study showed brain volume loss decreased during Phase 3
studies and was sustained with continuous Zeposia treatment for up
to 5 years
More than eight years of DAYBREAK data
confirm established safety profile of Zeposia, with rates of
treatment-emergent adverse events declining or stable over
time
Bristol Myers Squibb (NYSE: BMY) today announced new data from
the Phase 3 DAYBREAK trial demonstrating that decreased rates of
brain volume loss were sustained in the open-label extension (OLE)
for patients treated with Zeposia (ozanimod) for relapsing forms of
multiple sclerosis. These findings showed that patients receiving
continuous Zeposia treatment for up to five years experienced low
and stable rates of whole brain volume (WBV) loss through Month 60
(annualized least squares mean [LSM] % change from parent trial
baseline: RADIANCE, −0.27; SUNBEAM, −0.35).
Additionally, findings from a separate DAYBREAK OLE safety
analysis demonstrated declining or stable incidence rates of
treatment-emergent adverse events (TEAEs), with relatively low
rates of infections, serious infections and opportunistic
infections over more than eight years of treatment with
Zeposia.
These data and 12 additional abstracts will be presented at the
40th Congress of the European Committee for Treatment and Research
in Multiple Sclerosis (ECTRIMS) in Copenhagen, Denmark taking place
September 18-20, 2024.
“If not treated early upon diagnosis, multiple sclerosis can
lead to significant, irreversible brain volume loss and cognitive
decline,” said Jeffrey Cohen, MD, Mellen Center for Multiple
Sclerosis, Cleveland Clinic, Cleveland, Ohio and a paid consultant
for Bristol Myers Squibb. “These new analyses reinforce the
well-established safety and efficacy profile of Zeposia as an
effective oral therapy, especially for newly diagnosed patients
living with relapsing forms of multiple sclerosis.”
Reductions in brain volume loss with Zeposia treatment
The DAYBREAK OLE trial included 2,257 patients from the SUNBEAM
and RADIANCE Phase 3 trials and evaluated rates of brain volume
loss (Poster #P1623). Switching from interferon beta-1a (IFN-β) to
Zeposia treatment consistently reduced rates of WBV loss
(annualized LSM% change from RADIANCE baseline to Month 24 and
DAYBREAK baseline to Month 24: −0.48 and −0.19, respectively, with
a similar pattern observed in SUNBEAM). Additionally, similar
reductions were observed for change in thalamic volume loss.
High annualized LSM% reductions in cortical grey matter volume
(CGMV) were observed with IFN-β (annualized change at Month 12
relative to SUNBEAM baseline: −1.02; annualized change at Month 24
relative to RADIANCE baseline: −0.59), but this trend reversed 12
months after switching to Zeposia in DAYBREAK (annualized LSM%
increase relative to DAYBREAK baseline: patients from SUNBEAM,
0.10; patients from RADIANCE, 0.20), with low annualized LSM% CGMV
loss observed thereafter.
Established Zeposia safety profile confirmed with more than
eight years of DAYBREAK data
The final DAYBREAK OLE safety analysis (Poster #P1609) included
762 patients who were treated with continuous Zeposia with a median
exposure of 83.9 months. Incident rates per 1,000 person-years
decreased over time from the Phase 3 trials to Month 60 or more of
the DAYBREAK OLE trial. Decreases were observed for overall TEAEs
(896.1 versus 101.7), infections (300.5 versus 142.6),
opportunistic infections (12.0 versus 4.9), cardiac (22.8 versus
9.5), hepatic (77.0 versus 15.7) and pulmonary disorders (11.3
versus 4.7), respectively.
“The data presented at ECTRIMS further reinforce the long-term
safety and efficacy of Zeposia and add to the robust body of
evidence demonstrating its potential impact on decreasing disease
progression over time,” said Alyssa Johnsen, MD, PhD, senior vice
president and head of clinical development, Immunology,
Cardiovascular and Neuroscience, Bristol Myers Squibb. “Building on
our expertise with Zeposia, we are expanding our pipeline as we
continue to look for new ways to advance the field of neuroscience.
New modalities and disease targets fuel our goal of delivering
medicines that elevate standards of care across neurological
diseases, including multiple sclerosis.”
Bristol Myers Squibb thanks the patients and investigators who
participated in the Zeposia clinical trials.
About DAYBREAK
DAYBREAK was a Phase 3, multi-center, long-term open-label
extension study to evaluate the safety and efficacy of Zeposia
(ozanimod) administered orally to patients with relapsing forms of
multiple sclerosis (RMS).
Eligible patients from the RADIANCE, SUNBEAM and RPC01-1001
trials diagnosed with RMS were enrolled to receive treatment until
the end of the DAYBREAK. Patients in the trial received Zeposia
0.92 mg (equivalent to 1 mg).
About SUNBEAM
SUNBEAM was a pivotal, Phase 3, multicenter, randomized,
double-blind, double-dummy, active-controlled trial evaluating the
efficacy, safety and tolerability of two doses of oral Zeposia
(0.92 mg and 0.46 mg, equivalent to 1 mg and 0.5 mg, respectively)
against weekly intramuscular Avonex® for at least a 12-month
treatment period. The study included 1,346 people living with RMS
across 152 sites in 20 countries.
The primary endpoint of the trial was annualized relapse rates
during the treatment period. The secondary MRI endpoints included
the number of new or enlarging hyperintense T2-weighted brain MRI
lesions over 12 months, number of gadolinium-enhanced brain MRI
lesions at Month 12 and percent change from baseline in whole brain
volume at Month 12. Cortical grey and thalamic volume changes were
also prospectively assessed versus active comparator.
About RADIANCE
RADIANCE Part B was a pivotal, Phase 3, multicenter, randomized,
double-blind, double-dummy, active-controlled trial evaluating the
efficacy, safety and tolerability of oral Zeposia 0.92 mg
(equivalent to 1 mg) against weekly intramuscular Avonex®
(interferon beta-1a) over a 24-month treatment period. The study
included 1,320 people living with RMS across 150 sites in 21
countries.
The primary endpoint of the trial was annualized relapse rates
over 24 months. The secondary MRI endpoints included the number of
new or enlarging hyperintense T2-weighted brain MRI lesions over 24
months.
About Multiple Sclerosis
Multiple sclerosis (MS) is a disabling, unpredictable disease in
which the immune system attacks the protective myelin sheath that
covers the nerves. The myelin damage disrupts communication between
the brain and the rest of the body. Ultimately, the nerves
themselves may deteriorate—a process that's currently irreversible.
MS affects 700,000 people in Europe and approximately 2.9 million
people worldwide.
Relapsing forms of MS (RMS), including clinically isolated
syndrome, relapsing remitting disease and active secondary
progressive disease, is characterized by clearly defined attacks of
worsening neurologic function. These attacks—often called relapses,
flare-ups or exacerbations—are followed by partial or complete
recovery periods. During these recovery periods, also called
remissions, symptoms improve partially or completely with no
apparent progression of disease. However, smoldering
neuroinflammation can be present from the earliest stages of MS,
which is underlying and continuous disease activity occurring
simultaneously in different areas of the brain that contributes to
disability accumulation. Since MS relapses are unpredictable,
patients can feel frustrated, stressed or scared when they occur.
RMS is the most common disease course at the time of diagnosis.
Approximately 85% of patients are initially diagnosed with RMS,
compared with 10%-15% diagnosed with progressive forms of the
disease.
Bristol Myers Squibb: Delivering Breakthrough Science for
Meaningful Interventions in Neuroscience
Neurological conditions represent some of the greatest
challenges of our time because of their impact on society,
including patients, caregivers, families and healthcare systems. At
Bristol Myers Squibb, we are committed to advancing our robust
pipeline of potential medicines for neurological disorders with the
goal of modifying disease and improving quality of life. Leveraging
genetics, biomarkers and predictive sciences, we target key
pathways involved in the initiation and progression of neurological
diseases to develop therapies with the potential to optimize
patient outcomes.
About Zeposia (ozanimod)
Zeposia (ozanimod) is an oral, sphingosine 1-phosphate (S1P)
receptor modulator that binds with high affinity to S1P receptors 1
and 5. Zeposia blocks the capacity of lymphocytes to egress from
lymph nodes, reducing the number of lymphocytes in peripheral
blood. The mechanism by which Zeposia exerts therapeutic effects in
multiple sclerosis (MS) is unknown but may involve the reduction of
lymphocyte migration into the central nervous system.
Zeposia is approved in numerous countries around the world for
the treatment of adults with relapsing forms of MS and adults with
moderately to severely active ulcerative colitis.
U.S. FDA APPROVED INDICATIONS
ZEPOSIA® (ozanimod) is indicated for the treatment of:
- Relapsing forms of multiple sclerosis (MS), to include
clinically isolated syndrome, relapsing-remitting disease, and
active secondary progressive disease, in adults.
- Moderately to severely active ulcerative colitis (UC) in
adults.
IMPORTANT SAFETY INFORMATION
Contraindications:
- Patients who in the last 6 months, experienced myocardial
infarction, unstable angina, stroke, transient ischemic attack
(TIA), decompensated heart failure requiring hospitalization, or
Class III/IV heart failure or have a presence of Mobitz type II
second-degree or third-degree atrioventricular (AV) block, sick
sinus syndrome, or sino-atrial block, unless the patient has a
functioning pacemaker
- Patients with severe untreated sleep apnea
- Patients taking a monoamine oxidase (MAO) inhibitor
Infections: ZEPOSIA may increase the susceptibility to
infections. Life-threatening and rare fatal infections have
occurred in patients receiving ZEPOSIA. Obtain a recent (i.e.,
within 6 months or after discontinuation of prior MS or UC therapy)
complete blood count (CBC) including lymphocyte count before
initiation of ZEPOSIA. Delay initiation of ZEPOSIA in patients with
an active infection until the infection is resolved. Consider
interruption of treatment with ZEPOSIA if a patient develops a
serious infection. Continue monitoring for infections up to 3
months after discontinuing ZEPOSIA.
- Herpes zoster was reported as an adverse reaction in
ZEPOSIA-treated patients. Herpes simplex encephalitis and varicella
zoster meningitis have been reported with sphingosine 1-phosphate
(S1P) receptor modulators. Patients without a healthcare
professional-confirmed history of varicella (chickenpox), or
without documentation of a full course of vaccination against
varicella zoster virus (VZV), should be tested for antibodies to
VZV before initiating ZEPOSIA. A full course of vaccination for
antibody-negative patients with varicella vaccine is recommended
prior to commencing treatment with ZEPOSIA.
- Cases of fatal cryptococcal meningitis (CM) were reported in
patients treated with another S1P receptor modulator. If CM is
suspected, ZEPOSIA should be suspended until cryptococcal infection
has been excluded. If CM is diagnosed, appropriate treatment should
be initiated.
- In the MS and UC clinical studies, patients who received
ZEPOSIA were not to receive concomitant treatment with
antineoplastic, non-corticosteroid immunosuppressive, or
immune-modulating therapies used for treatment of MS and UC.
Concomitant use of ZEPOSIA with any of these therapies would be
expected to increase the risk of immunosuppression. When switching
to ZEPOSIA from immunosuppressive medications, consider the
duration of their effects and their mode of action to avoid
unintended additive immunosuppressive effects.
- Use of live attenuated vaccines should be avoided during and
for 3 months after treatment with ZEPOSIA. If live attenuated
vaccine immunizations are required, administer at least 1 month
prior to initiation of ZEPOSIA.
Progressive Multifocal Leukoencephalopathy (PML): PML is
an opportunistic viral infection of the brain that typically occurs
in patients who are immunocompromised, and that usually leads to
death or severe disability.
PML has been reported in patients treated with S1P receptor
modulators, including ZEPOSIA, and other MS and UC therapies and
has been associated with some risk factors. If PML is suspected,
withhold ZEPOSIA and perform an appropriate diagnostic
evaluation.
If confirmed, treatment with ZEPOSIA should be discontinued.
Immune reconstitution inflammatory syndrome (IRIS) has been
reported in MS patients treated with S1P receptor modulators who
developed PML and subsequently discontinued treatment. IRIS
presents as a clinical decline in the patient’s condition that may
be rapid, can lead to serious neurological complications or death,
and is often associated with characteristic changes on MRI. The
time to onset of IRIS in patients with PML was generally within a
few months after S1P receptor modulator discontinuation. Monitoring
for development of IRIS and appropriate treatment of the associated
inflammation should be undertaken.
Bradyarrhythmia and Atrioventricular Conduction Delays:
Since initiation of ZEPOSIA may result in a transient decrease in
heart rate and atrioventricular conduction delays, dose titration
is recommended to help reduce cardiac effects. Initiation of
ZEPOSIA without dose escalation may result in greater decreases in
heart rate. If treatment with ZEPOSIA is considered, advice from a
cardiologist should be sought for those individuals:
- with significant QT prolongation
- with arrhythmias requiring treatment with Class 1a or III
anti-arrhythmic drugs
- with ischemic heart disease, heart failure, history of cardiac
arrest or myocardial infarction, cerebrovascular disease, and
uncontrolled hypertension
- with a history of Mobitz type II second-degree or higher AV
block, sick sinus syndrome, or sino-atrial heart block
Liver Injury: Elevations of aminotransferases may occur
in patients receiving ZEPOSIA. Obtain liver function tests, if not
recently available (i.e., within 6 months), before initiation of
ZEPOSIA. Patients who develop symptoms suggestive of hepatic
dysfunction should have hepatic enzymes checked and ZEPOSIA should
be discontinued if significant liver injury is confirmed.
Fetal Risk: There are no adequate and well-controlled
studies in pregnant women. Based on animal studies, ZEPOSIA may
cause fetal harm. Women of childbearing potential should use
effective contraception to avoid pregnancy during treatment and for
3 months after stopping ZEPOSIA. Women who become pregnant while
taking ZEPOSIA for MS may enroll in the ZEPOSIA pregnancy registry
by calling 1-877-301-9314 or visiting
www.zeposiapregnancyregistry.com.
Increased Blood Pressure: Increase in systolic pressure
was observed after about 3 months of treatment and persisted
throughout treatment. Blood pressure should be monitored during
treatment and managed appropriately. Certain foods that may contain
very high amounts of tyramine could cause severe hypertension in
patients taking ZEPOSIA. Patients should be advised to avoid foods
containing a very large amount of tyramine while taking
ZEPOSIA.
Respiratory Effects: ZEPOSIA may cause a decline in
pulmonary function. Spirometric evaluation of respiratory function
should be performed during therapy, if clinically indicated.
Macular Edema: S1P modulators have been associated with
an increased risk of macular edema. Patients with a history of
uveitis or diabetes mellitus are at increased risk. Patients with a
history of these conditions should have an ophthalmic evaluation of
the fundus, including the macula, prior to treatment initiation and
regular follow-up examinations. An ophthalmic evaluation is
recommended in all patients at any time if there is a change in
vision. Continued use of ZEPOSIA in patients with macular edema has
not been evaluated; potential benefits and risks for the individual
patient should be considered if deciding whether ZEPOSIA should be
discontinued.
Posterior Reversible Encephalopathy Syndrome (PRES): Rare
cases of PRES have been reported in patients receiving a S1P
receptor modulator. If a ZEPOSIA-treated patient develops
unexpected neurological or psychiatric symptoms or any symptom/sign
suggestive of an increase in intracranial pressure, a complete
physical and neurological examination should be conducted. Symptoms
of PRES are usually reversible but may evolve into ischemic stroke
or cerebral hemorrhage. Delay in diagnosis and treatment may lead
to permanent neurological sequelae. If PRES is suspected, treatment
with ZEPOSIA should be discontinued.
Unintended Additive Immunosuppressive Effects From Prior
Immunosuppressive or Immune-Modulating Drugs: When switching
from drugs with prolonged immune effects, the half-life and mode of
action of these drugs must be considered to avoid unintended
additive immunosuppressive effects while at the same time
minimizing risk of disease reactivation. Initiating treatment with
ZEPOSIA after treatment with alemtuzumab is not recommended.
Severe Increase in Multiple Sclerosis (MS) Disability After
Stopping ZEPOSIA: In MS, severe exacerbation of disease,
including disease rebound, has been rarely reported after
discontinuation of a S1P receptor modulator. The possibility of
severe exacerbation of disease should be considered after stopping
ZEPOSIA treatment so patients should be monitored upon
discontinuation. After stopping ZEPOSIA in the setting of PML,
monitor for development of immune reconstitution inflammatory
syndrome (PML-IRIS).
Immune System Effects After Stopping ZEPOSIA: After
discontinuing ZEPOSIA, the median time for lymphocyte counts to
return to the normal range was 30 days with approximately 90% of
patients in the normal range within 3 months. Use of
immunosuppressants within this period may lead to an additive
effect on the immune system, therefore caution should be applied
when initiating other drugs 4 weeks after the last dose of
ZEPOSIA.
Most Common Adverse Reactions that occurred in the MS
clinical trials of ZEPOSIA-treated patients (≥4%): upper
respiratory infection, hepatic transaminase elevation, orthostatic
hypotension, urinary tract infection, back pain, and
hypertension.
In the UC clinical trials, the most common adverse reactions
that occurred in ≥4% of ZEPOSIA-treated patients and greater than
in patients who received placebo were upper respiratory infection,
liver test increased, and headache.
Use in Specific Populations: Hepatic Impairment: Dosage
adjustment in patients with mild or moderate hepatic impairment
(Child-Pugh class A or B) is required, and use of ZEPOSIA in
patients with severe hepatic impairment (Child-Pugh class C) is not
recommended.
For additional safety information, please see the full
Prescribing Information and Medication
Guide.
About Bristol Myers Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose
mission is to discover, develop and deliver innovative medicines
that help patients prevail over serious diseases. For more
information about Bristol Myers Squibb, visit us at BMS.com or
follow us on LinkedIn, Twitter, YouTube, Facebook and
Instagram.
Cautionary Statement Regarding Forward-Looking
Statements
This press release contains “forward-looking statements” within
the meaning of the Private Securities Litigation Reform Act of 1995
regarding, among other things, the research, development and
commercialization of pharmaceutical products. All statements that
are not statements of historical facts are, or may be deemed to be,
forward-looking statements. Such forward-looking statements are
based on current expectations and projections about our future
financial results, goals, plans and objectives and involve inherent
risks, assumptions and uncertainties, including internal or
external factors that could delay, divert or change any of them in
the next several years, that are difficult to predict, may be
beyond our control and could cause our future financial results,
goals, plans and objectives to differ materially from those
expressed in, or implied by, the statements. These risks,
assumptions, uncertainties and other factors include, among others,
that results of future post-marketing studies will be consistent
with the results of this study, that Zeposia (ozanimod) for the
indication described in this release may not be commercially
successful, any marketing approvals, if granted, may have
significant limitations on their use, and that continued approval
of Zeposia for such indication may be contingent upon verification
and description of clinical benefit in additional confirmatory
trials. No forward-looking statement can be guaranteed.
Forward-looking statements in this press release should be
evaluated together with the many risks and uncertainties that
affect Bristol Myers Squibb’s business and market, particularly
those identified in the cautionary statement and risk factors
discussion in Bristol Myers Squibb’s Annual Report on Form 10-K for
the year ended December 31, 2023, as updated by our subsequent
Quarterly Reports on Form 10-Q, Current Reports on Form 8-K and
other filings with the Securities and Exchange Commission. The
forward-looking statements included in this document are made only
as of the date of this document and except as otherwise required by
applicable law, Bristol Myers Squibb undertakes no obligation to
publicly update or revise any forward-looking statement, whether as
a result of new information, future events, changed circumstances
or otherwise.
corporatefinancial-news
View source
version on businesswire.com: https://www.businesswire.com/news/home/20240917429806/en/
Bristol Myers Squibb Media Inquiries:
media@bms.com Investors: investor.relations@bms.com
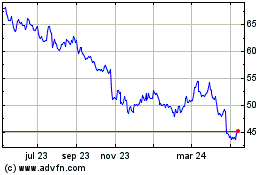
Bristol Myers Squibb (NYSE:BMY)
Gráfica de Acción Histórica
De Nov 2024 a Dic 2024
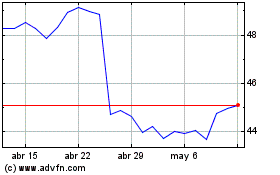
Bristol Myers Squibb (NYSE:BMY)
Gráfica de Acción Histórica
De Dic 2023 a Dic 2024